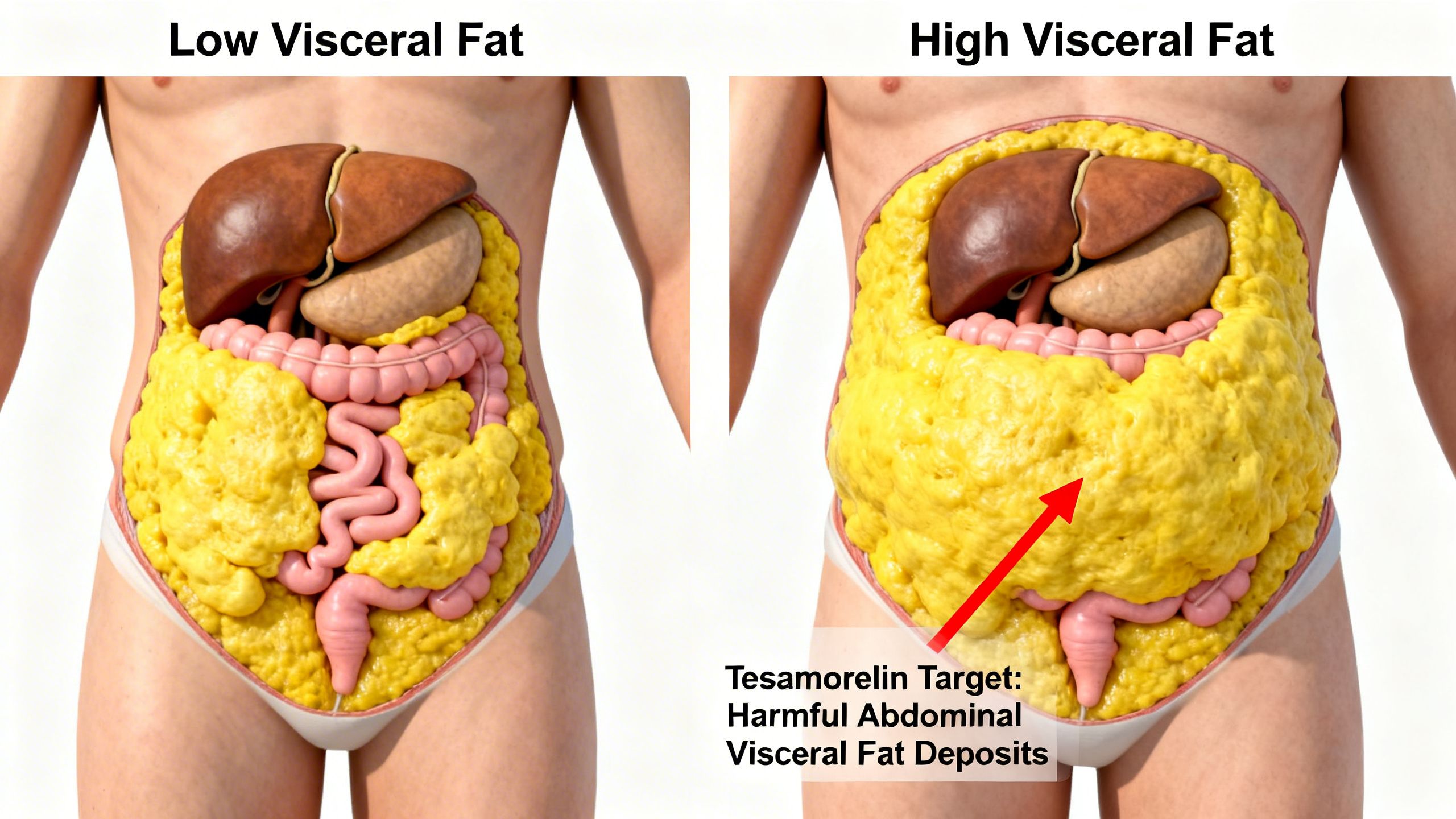
Visceral fat, the deep abdominal fat that surrounds vital organs, is a significant contributor to metabolic disease, inflammation, and cardiovascular risk. Unlike subcutaneous fat, which lies just beneath the skin, visceral adipose tissue (VAT) is metabolically active and notoriously difficult to lose through diet and exercise alone. In the search for targeted therapeutic interventions, the Tesamorelin peptide has emerged as a powerful and well-researched compound, primarily recognized for its ability to selectively reduce this dangerous fat while also influencing overall body composition and muscle health.
Originally developed and FDA-approved to treat excess abdominal fat in HIV-infected patients with lipodystrophy, Tesamorelin’s unique mechanism of action has garnered significant interest for broader applications related to aging and metabolic dysfunction. By stimulating the body’s own production of growth hormone in a controlled, physiological manner, it offers a distinct alternative to direct hormone replacement. This article provides a comprehensive, evidence-based exploration of what Tesamorelin is, its mechanism of action, the human clinical data supporting its use for visceral fat reduction, its effects on muscle health, and its safety profile.
What is Tesamorelin? A Deeper Look
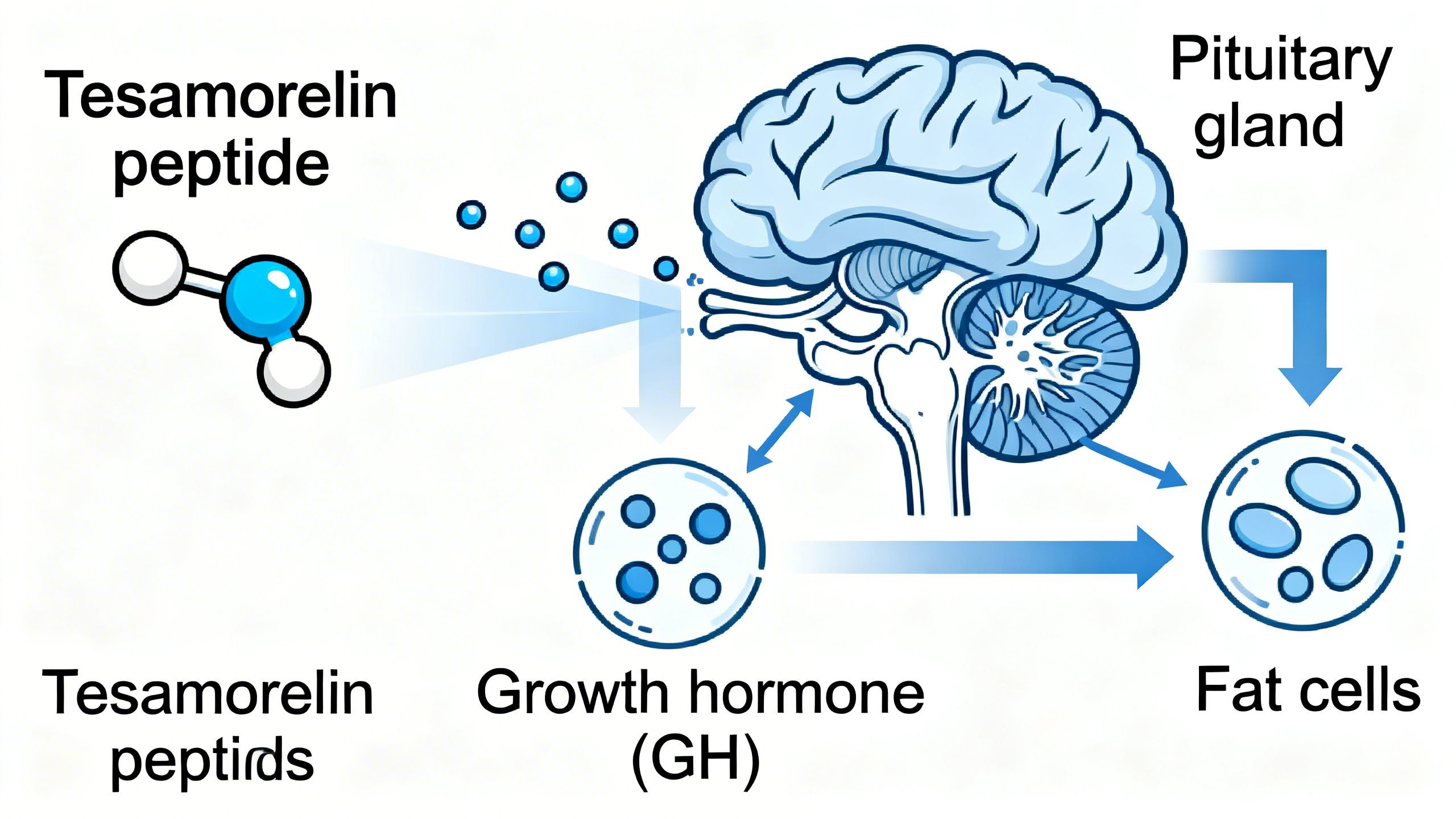
Tesamorelin is a synthetic peptide, which means it is a small protein made of a specific sequence of amino acids. It is classified as a growth hormone-releasing hormone (GHRH) analog. Endogenous GHRH is a hormone naturally produced in the hypothalamus of the brain, and its primary role is to signal the pituitary gland to produce and release growth hormone (GH).
Tesamorelin was engineered to mimic the action of natural GHRH. It consists of the same 44-amino acid chain as human GHRH but includes a specific modification (a trans-3-hexenoyl group) at one end. This structural alteration makes the peptide more stable and resistant to enzymatic degradation in the bloodstream. The result is a longer half-life and a more sustained effect compared to its natural counterpart, allowing for effective once-daily administration.
Crucially, Tesamorelin is not growth hormone itself. Instead, it is a secretagogue—a substance that causes another substance to be secreted. By stimulating the pituitary gland, it promotes the release of the body’s own GH stores. This process preserves the natural pulsatile rhythm of GH secretion, which is characterized by periodic bursts of release, primarily during sleep. This pulsatility is believed to be critical for the hormone’s beneficial effects while potentially mitigating some of the side effects associated with the continuous high levels seen with direct injections of recombinant human growth hormone (rhGH).
The Mechanism of Action: How Tesamorelin Works
The therapeutic effects of the Tesamorelin peptide are mediated through the complex and elegant growth hormone axis, also known as the somatotropic axis. Understanding this pathway is key to appreciating how it achieves its targeted effects on fat and muscle.
- Pituitary Stimulation: After subcutaneous injection, Tesamorelin travels through the bloodstream to the anterior pituitary gland. There, it binds to specific GHRH receptors on the surface of pituitary cells called somatotrophs. This binding is the primary trigger for the synthesis and release of growth hormone.
- Pulsatile GH Release: The stimulation from Tesamorelin results in a significant, yet pulsatile, increase in circulating GH levels. This mimics the body’s natural pattern of GH release, avoiding the constant, supraphysiological levels that can disrupt metabolic feedback loops.
- IGF-1 Production: The released growth hormone then travels to the liver, its primary target organ. In the liver, GH stimulates the production and secretion of another crucial hormone: Insulin-like Growth Factor 1 (IGF-1). IGF-1 is a primary mediator of many of GH’s anabolic (tissue-building) and metabolic effects throughout the body.
- Tesamorelin Fat Loss Mechanism: The increased levels of both GH and IGF-1 initiate powerful metabolic changes. Specifically for fat loss, GH has a direct lipolytic effect. It binds to receptors on adipocytes (fat cells), particularly visceral fat cells, and triggers the breakdown of stored triglycerides into free fatty acids and glycerol. These fatty acids are then released into the bloodstream to be used as energy by other tissues, leading to a net reduction in fat mass.
- Anabolic Effects on Muscle: Simultaneously, IGF-1 and GH exert anabolic effects on muscle tissue. They promote the uptake of amino acids by muscle cells and stimulate the mTOR pathway, a central regulator of cell growth and protein synthesis. This leads to an increase in lean body mass and can improve muscle strength and function.
This dual-action mechanism—promoting lipolysis in visceral fat while supporting anabolism in muscle—is what makes Tesamorelin a compelling agent for improving body composition.
Tesamorelin for Visceral Fat: Reviewing the Human Evidence
The most robust clinical evidence for Tesamorelin’s efficacy comes from large-scale, randomized, placebo-controlled trials in HIV-infected patients with lipodystrophy, a condition characterized by abnormal fat distribution, including the accumulation of visceral fat. These studies were pivotal for its FDA approval.
In two landmark Phase 3 trials, patients receiving a daily 2 mg injection of Tesamorelin for 26 weeks experienced a statistically significant reduction in visceral adipose tissue (VAT) compared to placebo. The average reduction was approximately 15-18%, a clinically meaningful outcome given the metabolic risks associated with VAT. Importantly, these studies showed that Tesamorelin selectively targeted visceral fat, with minimal to no effect on beneficial subcutaneous fat.
An extension phase of these studies demonstrated that continued treatment for up to 52 weeks led to sustained reductions in VAT. However, it was also observed that upon cessation of treatment, VAT levels began to return toward baseline, suggesting that ongoing therapy is necessary to maintain the benefits. This finding underscores that Tesamorelin is a treatment, not a cure, for visceral fat accumulation.
Beyond the HIV population, research has explored its potential in other groups. A study in non-HIV individuals with abdominal obesity also showed that Tesamorelin significantly reduced VAT and improved lipid profiles, including a reduction in triglycerides and total cholesterol. These findings suggest that the tesamorelin for visceral fat benefits are not limited to a specific disease state but are a direct result of its mechanism of action on the GH axis.
Tesamorelin and Muscle Health: Beyond Fat Loss
While visceral fat reduction is its primary claim to fame, the anabolic effects of the GH/IGF-1 axis mean that tesamorelin and muscle health are closely linked. The stimulation of muscle protein synthesis and the potential to increase lean body mass are significant secondary benefits observed in clinical trials.
In the same pivotal studies of HIV patients, participants treated with Tesamorelin showed modest but statistically significant increases in lean body mass. While the primary endpoint was fat reduction, these changes in body composition are highly relevant. An increase in muscle mass can improve metabolic rate, enhance physical function, and contribute to overall health and resilience.
Further research has specifically investigated muscle-related outcomes. One study examined the effects of Tesamorelin on muscle fat infiltration and muscle density in the HIV population. The results indicated that Tesamorelin not only reduced visceral fat but also decreased the amount of fat within the muscle tissue itself, a condition known as myosteatosis, which is associated with poor muscle quality and insulin resistance. The treatment also led to an increase in muscle density, a proxy for improved muscle quality.
These findings suggest a potential role for Tesamorelin in combating age-related muscle loss (sarcopenia) or other conditions characterized by a decline in muscle mass and function. By promoting a more favorable hormonal environment for muscle growth and maintenance, Tesamorelin could be a valuable tool for improving overall tesamorelin body composition and physical performance, although more research is needed in non-HIV, aging populations to confirm these benefits.
Tesamorelin Dosage and Administration
Understanding the proper tesamorelin dosage and administration is critical for safety and efficacy. The clinically studied and FDA-approved dosage for the treatment of HIV-associated lipodystrophy is 2 mg of Tesamorelin administered once daily.
Administration Details:
- Method: Tesamorelin is administered via subcutaneous injection, meaning it is injected into the fatty layer of tissue just under the skin.
- Site: The abdomen is the recommended injection site. It is important to rotate injection sites daily to avoid lipohypertrophy (a lump under the skin caused by an accumulation of extra fat) or other site reactions.
- Reconstitution: The peptide comes as a lyophilized (freeze-dried) powder that must be reconstituted with sterile water for injection, which is provided with the medication. Careful adherence to the reconstitution instructions is essential to ensure the correct concentration and sterility.
- Timing: While it can be administered at any time of day, some practitioners recommend taking it before bedtime to mimic the natural nocturnal peak of growth hormone release.
It is crucial to emphasize that this information is for educational purposes only and does not constitute medical advice. The appropriate dosage and treatment plan must be determined by a qualified healthcare professional based on an individual’s medical history, diagnosis, and lab results. Using a generic tesamorelin dosage chart or tesamorelin dosage calculator found online is strongly discouraged and can be dangerous.
Potential Side Effects and Safety Profile
Like any therapeutic agent, Tesamorelin is associated with a range of potential side effects. The majority are mild to moderate and are related to the increase in GH and IGF-1 levels, which can cause fluid retention and tissue growth.
Common Tesamorelin Side Effects:
- Injection Site Reactions: Redness, pain, itching, and swelling at the injection site are the most frequently reported side effects.
- Arthralgia (Joint Pain): Increased fluid retention can lead to stiffness and pain in the joints.
- Myalgia (Muscle Pain): Aches and pains in the muscles can occur.
- Peripheral Edema: Swelling in the extremities, such as the hands and feet, due to fluid retention.
- Paresthesia: Sensations of numbness or tingling, often associated with carpal tunnel-like symptoms.
Less Common but More Serious Concerns:
- Glucose Intolerance: Increased GH levels can induce insulin resistance. Therefore, blood glucose and hemoglobin A1c levels should be monitored, especially in patients with pre-existing diabetes or prediabetes. Individuals with poorly controlled diabetes may need to adjust their medication.
- Increased IGF-1 Levels: The therapy directly increases IGF-1. While the long-term risks are not fully established, elevated IGF-1 is theoretically linked to an increased risk of certain malignancies. For this reason, Tesamorelin is contraindicated in patients with active cancer.
- Hypersensitivity Reactions: Although rare, allergic reactions, including rash and urticaria (hives), can occur.
Patients should always discuss their full medical history with their doctor before starting treatment. A thorough evaluation is necessary to weigh the potential benefits against the risks.

Comparing Tesamorelin to Other Compounds
To fully understand Tesamorelin’s place in therapeutics, it’s helpful to compare it to other related compounds that influence the growth hormone axis.
Sermorelin vs Tesamorelin
Sermorelin is another GHRH analog, but it represents only the first 29 amino acids of the GHRH sequence. Tesamorelin contains the full 44-amino acid sequence plus a stabilizing modification. This structural difference makes Tesamorelin significantly more potent and stable, with a longer half-life. As a result, Tesamorelin produces a more robust and sustained release of GH and increase in IGF-1 compared to Sermorelin, which is why it has demonstrated superior efficacy in reducing visceral fat in head-to-head clinical contexts.
Tesamorelin vs. Ipamorelin and other GHRPs
Ipamorelin belongs to a different class of secretagogues called Growth Hormone Releasing Peptides (GHRPs). These compounds work by mimicking the hormone ghrelin and binding to the GHS-R1a receptor in the pituitary. This is a separate mechanism from Tesamorelin’s action on the GHRH receptor. While both stimulate GH release, they do so through different pathways. Some protocols involve combining a GHRH analog with a GHRP for a potentially synergistic effect, but robust human data on the long-term safety and efficacy of such combinations is limited.
Tesamorelin vs. Recombinant Growth Hormone (rhGH)
This is a critical distinction. Administering rhGH involves injecting exogenous growth hormone directly into the body, leading to consistently high, non-pulsatile levels. In contrast, the Tesamorelin peptide stimulates the body’s own pituitary to release GH in a pulsatile fashion. This physiological release pattern is thought to reduce the risk of side effects like insulin resistance and edema, which are more common with rhGH therapy. Furthermore, Tesamorelin preserves the integrity of the pituitary feedback loop, whereas long-term rhGH use can suppress natural GH production.
Role of IGF-1 and Metformin
IGF-1 is not a secretagogue but the downstream effector of GH. Monitoring its levels is a key part of therapy to ensure they remain within a safe and effective range. Metformin, a first-line medication for type 2 diabetes, is sometimes mentioned in the context of GH-stimulating therapies. It can be used to counteract the potential for insulin resistance that may arise from elevated GH levels, making it a potentially useful adjunct for managing metabolic side effects in some individuals.
Practical Considerations and Future Research
For those considering this therapy, managing expectations is key. The tesamorelin before and after results are not instantaneous. Clinical trials show that measurable reductions in visceral fat typically take several months to become apparent. The benefits are also contingent on consistent, daily administration. For optimal results, therapy should be combined with a healthy lifestyle, including a balanced diet and regular exercise.

The future of Tesamorelin research is promising. Studies are currently underway or have been completed exploring its potential benefits in other areas, including:
- Non-alcoholic fatty liver disease (NAFLD): By reducing visceral and liver fat, Tesamorelin may improve liver health.
- Mild Cognitive Impairment (MCI): Some research suggests that GH and IGF-1 play a role in neuronal health, and studies have investigated whether Tesamorelin can improve cognitive function in older adults.
- General Abdominal Obesity: More research is needed to establish its risk-benefit profile for visceral fat reduction in the general population without HIV.
Conclusion: The Role of Tesamorelin Peptide in Modern Therapeutics
The Tesamorelin peptide stands out as a highly effective and specific therapeutic agent for reducing visceral adipose tissue. Its mechanism of action—stimulating a physiological, pulsatile release of endogenous growth hormone—differentiates it from direct growth hormone administration and underpins its targeted effects and safety profile. The robust human evidence from large-scale clinical trials solidifies its efficacy in treating HIV-associated lipodystrophy, and emerging research continues to explore its potential for improving metabolic health, body composition, and even cognitive function in broader populations.
While its benefits for visceral fat loss and potential for enhancing muscle health are clear, it is not without side effects and requires careful medical supervision. As our understanding of metabolic disease and aging evolves, the Tesamorelin peptide represents a sophisticated tool for addressing some of the most challenging aspects of modern health, offering a targeted approach to improving body composition and reducing cardiometabolic risk.
Studies / References
- Tesamorelin reduces visceral fat and liver fat in HIV patients
Stanley TL, Feldpausch MN, Oh J, et al.
Effect of tesamorelin on visceral fat and liver fat in HIV-infected patients with abdominal fat accumulation: A randomized clinical trial. JAMA.
https://pubmed.ncbi.nlm.nih.gov/25038357/ - Meta-analysis of body composition and safety outcomes
Badran AS, Helal A, Shata KS, et al.
Body composition, hepatic fat, metabolic, and safety outcomes of tesamorelin in HIV-associated lipodystrophy: A meta-analysis of randomized controlled trials. Obes Res Clin Pract.
https://pubmed.ncbi.nlm.nih.gov/41545261/ - Early evidence of visceral fat reduction and sustained effects
Effects of tesamorelin in HIV-infected patients with abdominal fat accumulation: randomized trial with safety extension.
https://pubmed.ncbi.nlm.nih.gov/20101189/ - Reduction in visceral adiposity linked to metabolic improvements
Reduction in visceral adiposity is associated with an improved metabolic profile in HIV-infected patients receiving tesamorelin.
https://pubmed.ncbi.nlm.nih.gov/22495074/ - Expert review of tesamorelin use in HIV lipodystrophy
Mateo MG, Gutiérrez MDM, Domingo P.
Tesamorelin for the treatment of excess abdominal fat in HIV-1-infected patients with lipodystrophy. Expert Rev Endocrinol Metab.
https://pubmed.ncbi.nlm.nih.gov/30764032/ - Review article summarizing tesamorelin efficacy
Dhillon S.
Spotlight on tesamorelin in HIV-associated lipodystrophy. BioDrugs.
https://pubmed.ncbi.nlm.nih.gov/22050344/