Sarcopenia is a progressive and generalized skeletal muscle disorder that commonly affects older adults. It has profound impacts on mobility, independence, and overall quality of life, emerging as a major concern within the field of muscle health and aging. This article delves deeply into the mechanisms, research findings, diagnostic criteria, and evolving management strategies for sarcopenia, while highlighting human studies and cutting-edge interventions like peptides and hormone therapies.
Introduction: The Challenge of Sarcopenia in Older Adults
Sarcopenia refers to the age-related loss of muscle mass, strength, and function. It is more than just physical decline — sarcopenia in older adults is closely linked to frailty, increased falls, disability, and mortality. Recent research emphasizes the urgency to understand, diagnose, and counteract this condition as populations worldwide age.
Defining Sarcopenia: Criteria and Diagnosis
The official definition of sarcopenia has evolved. Modern guidelines, such as the European Working Group on Sarcopenia in Older People (EWGSOP2), recommend diagnosing based on:
- Low muscle strength (often measured by grip strength)
- Low muscle quantity or quality (assessed through imaging or bioimpedance)
- Low physical performance (gait speed, chair stand test)
Diagnostic Tools for Sarcopenia
| Assessment | Method | Typical Cut-off Values |
|---|---|---|
| Grip Strength | Hand dynamometer | <27 kg (men), <16 kg (women) |
| Muscle Mass | DXA, MRI, BIA | <7.0 kg/m² (men), <5.5 kg/m² (women) |
| Gait Speed | Timed walk test | <0.8 m/s |
Caveat: Body habitus, hydration, comorbidities, and ethnic background can influence test results and should be considered in assessment.
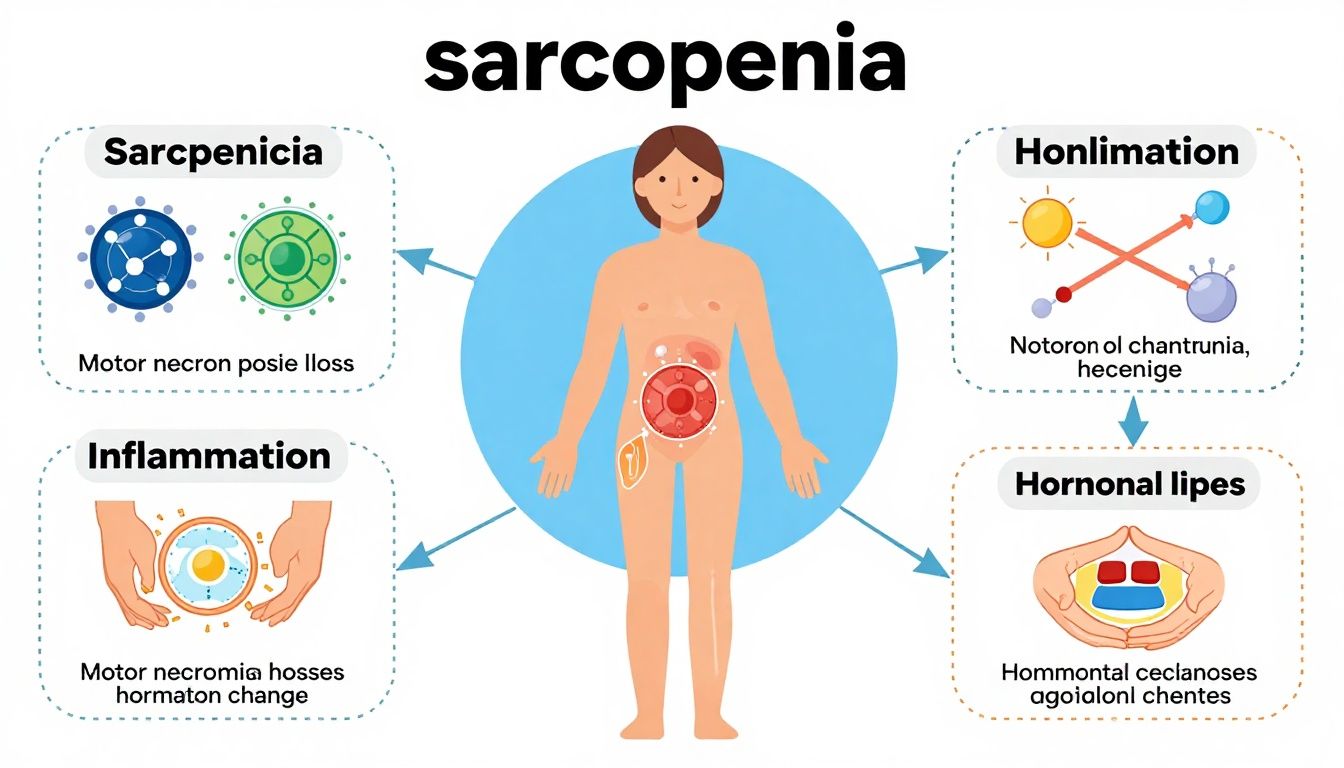
Mechanisms: Why Does Muscle Decline with Age?
The biology of sarcopenia is multifactorial. Key mechanisms include:
- Motor Neuron Loss: Aging depletes motor neurons, leading to muscle fiber denervation atrophy.
- Anabolic Resistance: Older adults’ muscles respond less efficiently to protein intake and exercise.
- Hormonal Changes: Declining levels of hormones like testosterone influence muscle synthesis.
- Inflammation: Chronic low-level inflammation (inflammaging) contributes to muscle catabolism.
- Physical Inactivity: Sedentary lifestyle accelerates muscle decline.
Genetics, nutrition, acute illness, and medication use further modulate risk.
Prevalence, Variability, and Risk Factors
Sarcopenia affects an estimated 10% to 20% of those over age 60, but prevalence varies widely depending on diagnostic criteria and population:
- Women and men are both at risk, though men lose more absolute muscle mass.
- Those with chronic disease, malnutrition, or inflammation face substantially increased risk.
- Recent studies observe notable differences in sarcopenia progression between ethnic groups, underscoring the impact of genetics and environmental factors.
Table: Major Risk Factors for Sarcopenia
| Factor | Details / Examples |
|---|---|
| Age | Over 60 years |
| Inactivity | Bed rest, sedentary lifestyle |
| Chronic Illness | Diabetes, COPD, heart failure |
| Poor Nutrition | Low protein/energy intake |
| Hormonal Changes | Low testosterone, estrogen, growth hormone |
| Inflammation | Increased CRP, IL-6 levels |
| Medications | Corticosteroids, statins |
Clinical Impact: From Muscle Loss to Frailty and Disability
The consequences of sarcopenia extend beyond reduced muscle size:
- Increased risk of falls and fractures
- Impaired ability to perform activities of daily living
- Higher hospitalization and institutionalization rates
- Increased mortality risk
Early identification and intervention can substantially improve trajectories for older adults.
Research Summary: Human Evidence on Sarcopenia
Decades of human research inform our understanding of sarcopenia’s origins, natural history, and modifiable factors.
- Large cohort studies reveal lifestyle, nutrition, and chronic disease as central modifiers of risk.
- Trials indicate that targeted exercise and optimized nutrition are effective primary interventions.
- Interest in pharmacological and peptide therapies, such as ostarine, BPC-157, and testosterone, is growing due to their anabolic effects in muscle tissue.
Interventions: Clinical Management and Emerging Therapies
Lifestyle and Exercise Strategies
Exercise is the cornerstone intervention for sarcopenia in older adults. Evidence supports:
- Progressive resistance training (2–3 times per week) for enhancing muscle mass and function
- Balance and flexibility training to reduce falls
- Aerobic conditioning for general health
Key Tip: Combination programs (resistance + balance + aerobic) provide the greatest functional improvements.
Nutritional Approaches
Optimizing nutrition is crucial. Focus on:
- Adequate protein intake (1.2–1.5 g/kg/day for older adults)
- Leucine-rich foods (dairy, eggs, whey), which are potent muscle protein synthesis stimulators
- Vitamin D status, as deficiency accelerates muscle loss

Compounds and Innovative Interventions
Interest in clinical compounds for sarcopenia has increased. Although robust, long-term human research is limited, three notable candidates include:
1. Ostarine (Enobosarm; SARM)
- Mechanism: Selective androgen receptor modulation enhances muscle protein synthesis with less androgenic side effects than testosterone.
- Human evidence: Clinical trials in older adults and cancer cachexia populations reveal moderate increases in lean body mass and grip strength, though benefits on function and long-term safety require further study.
2. BPC-157 (Peptide)
- Mechanism: Proposed effects on tissue repair, angiogenesis, and inflammation modulation. Limited human research, primarily small-scale studies.
- Evidence: Lacks robust placebo-controlled human trials in sarcopenia. Mentioned as a research target.
3. Testosterone (Hormone Replacement)
- Mechanism: Directly stimulates anabolic pathways in muscle; may also improve motivation and physical activity.
- Human evidence: Randomized trials show significant improvements in muscle mass and some strength/function indices, but potential risks include cardiovascular, prostate, and hematological side effects.
Medical caveat: All pharmacologic interventions for sarcopenia should be considered investigational. Approaches must be individualized and monitored by medical professionals.
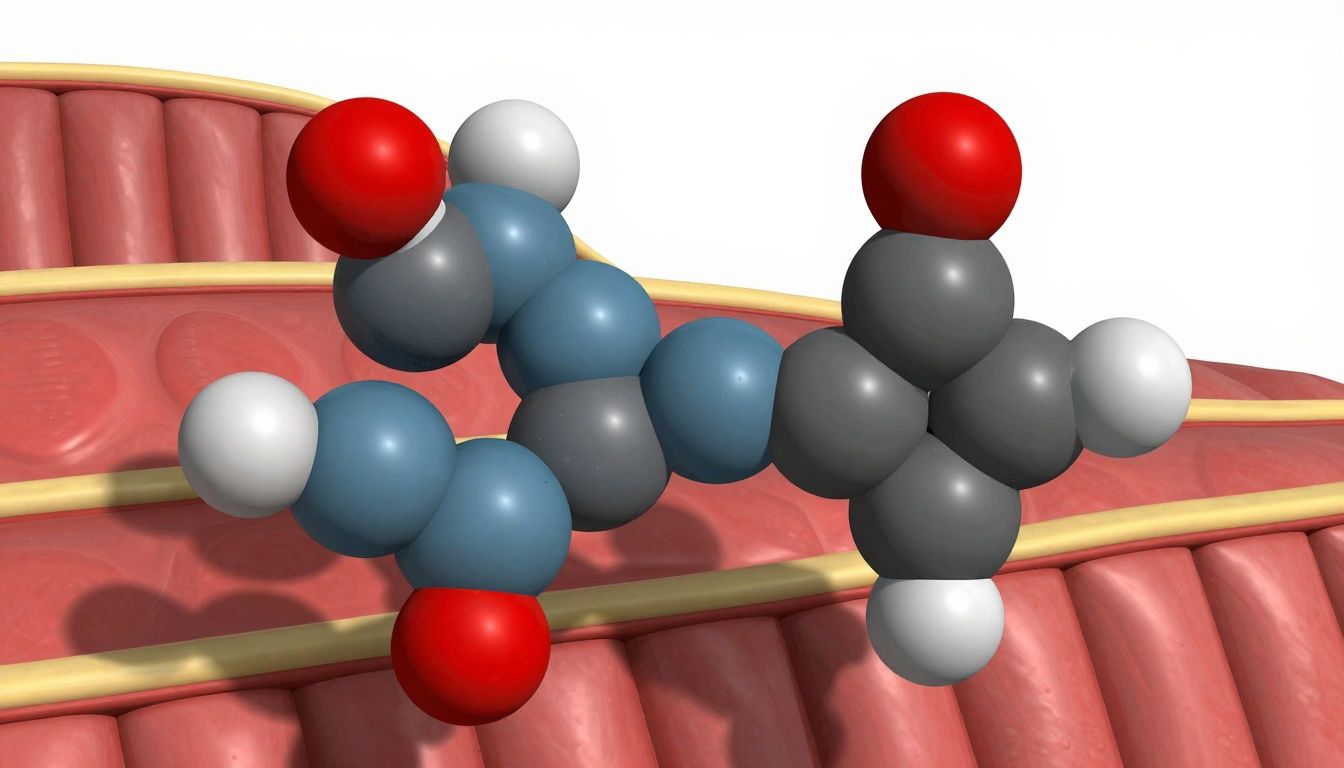
Table: Potential Effects of Suggested Compounds for Sarcopenia
| Compound | Reported Human Effects | Known Risks / Considerations |
|---|---|---|
| Ostarine | ↑ lean mass, ↑ some strength | Liver, lipid changes; unapproved use |
| BPC-157 | Limited human data; repair focus | Insufficient data |
| Testosterone | ↑ mass, ↑ strength, variable function | Polycythemia, prostate, CV risk |
Variability: Individual Responses and Personalized Approaches
The trajectory of sarcopenia and responses to interventions vary widely. Factors contributing to this variability include:
- Comorbidities: Chronic disease affects both muscle biology and therapy risks.
- Genetic background: Influences baseline muscle, injury repair, and responsiveness to anabolic agents.
- Activity and Diet Patterns: Interact with all interventions, often determining overall effectiveness.
Personalized care plans are essential, integrating multimodal strategies and safely considering experimental compounds where appropriate.
The Road Ahead: Research Gaps and Future Directions
Key areas for future investigation on sarcopenia include:
- Robust, long-term human trials for new compounds, including SARMs and specific peptides
- Optimized combined interventions (exercise + nutrition + pharmacology)
- Real-world studies of sarcopenia prevention
- Refinement of diagnostic criteria for diverse populations
Conclusion: Taking Action Against Sarcopenia
Sarcopenia is a common, impactful aspect of aging that underpins much of the frailty observed in older adults. Prompt recognition, comprehensive assessment, and evidence-based interventions — primarily resistance exercise and tailored nutrition — remain best practice. Peptides for sarcopenia, SARMs like ostarine, and even hormone therapies show promise, but require further human research and clinical caution.
Empowering older adults through proactive management of sarcopenia offers the best opportunity to maintain independence, mobility, and quality of life well into advanced age.