Retinal degenerative diseases, such as age-related macular degeneration (AMD) and retinitis pigmentosa, represent a formidable challenge in modern medicine, leading to progressive vision loss and affecting millions worldwide. The retina, a complex neural tissue at the back of the eye, has limited capacity for self-repair, making damage from these conditions largely irreversible with current standard treatments. In the quest for novel therapeutic strategies, the field of regenerative medicine has turned its attention to bioactive peptides—short chains of amino acids that act as powerful signaling molecules. The potential of retinal peptides to protect, repair, and possibly even regenerate damaged retinal tissue is a subject of intense scientific investigation, offering a glimmer of hope for conditions once deemed untreatable.
This article delves into the scientific landscape of peptides for eye health, with a specific focus on retinal regeneration. We will explore the mechanisms behind retinal degeneration, examine the evidence for specific compounds like GHK-Cu, BPC-157, and Thymosin Beta-4, and critically evaluate the human research available. Our goal is to provide a clear, evidence-based overview of what is known, what is hypothesized, and what remains to be discovered in this cutting-edge area of medical research.
The Challenge of Retinal Degeneration
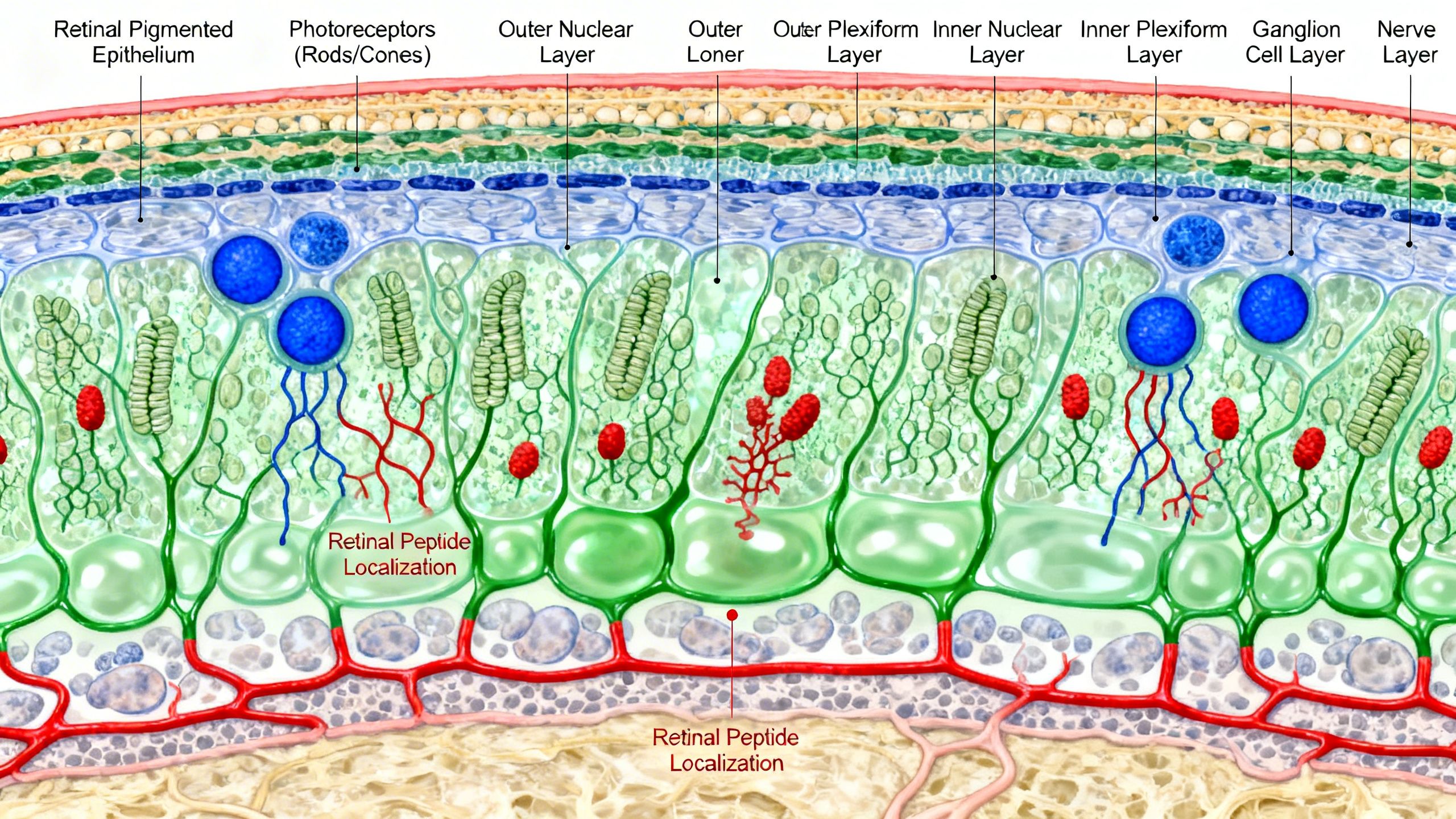
The retina is responsible for converting light into neural signals that the brain interprets as vision. It is composed of multiple layers of specialized cells, including photoreceptors (rods and cones) and retinal pigment epithelium (RPE) cells, which are crucial for its function and survival. Retinal degenerative diseases disrupt this delicate architecture.
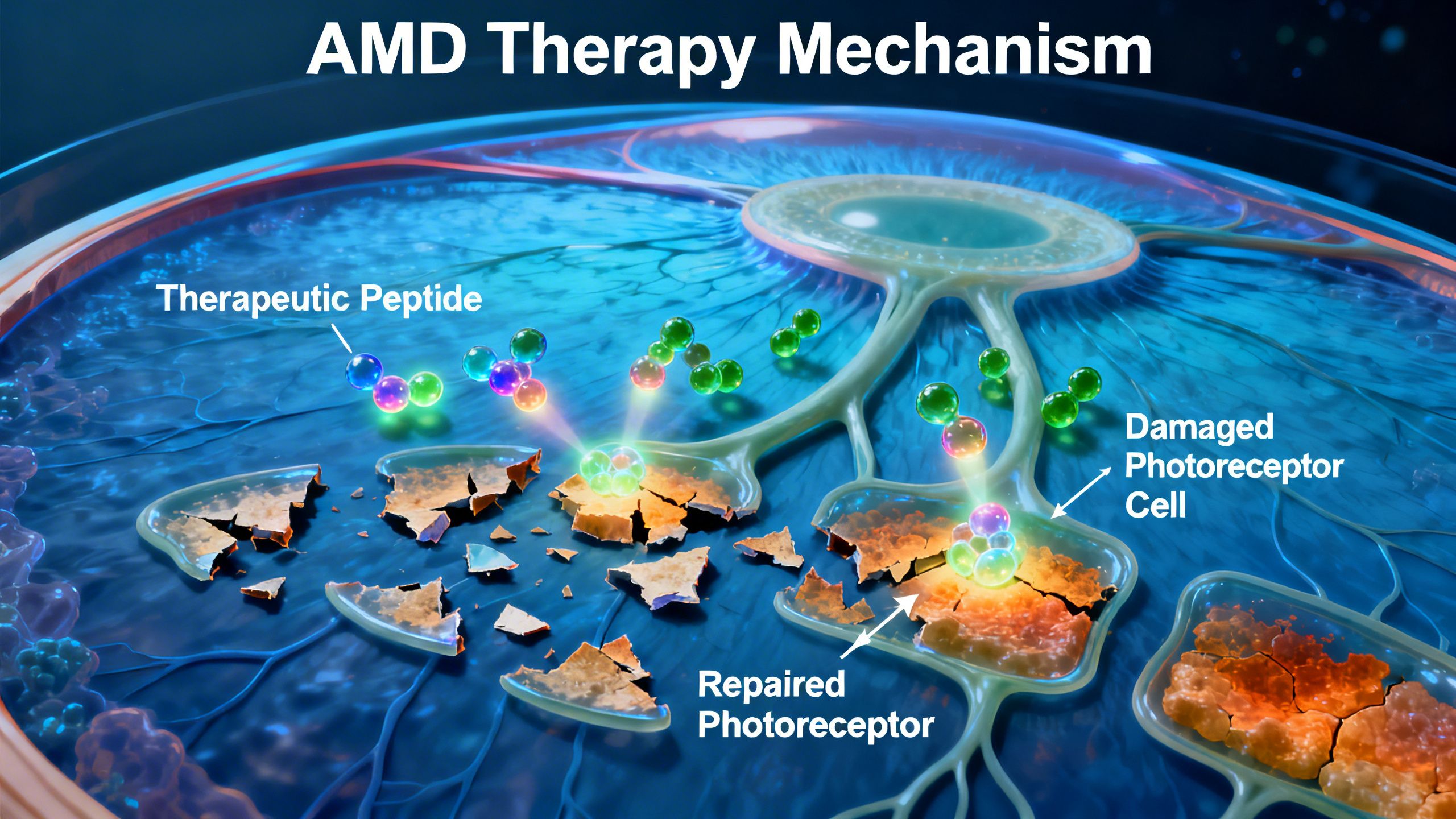
- Age-Related Macular Degeneration (AMD): This is the leading cause of severe vision loss in older adults. It primarily affects the macula, the central part of the retina responsible for sharp, detailed vision. AMD comes in two forms: the “dry” form, characterized by the accumulation of cellular debris (drusen) and gradual atrophy of RPE cells and photoreceptors, and the “wet” form, involving the growth of abnormal, leaky blood vessels that cause rapid and severe damage.
- Diabetic Retinopathy: A common complication of diabetes, this condition results from damage to the retinal blood vessels. It can lead to fluid leakage, swelling (macular edema), and the growth of fragile new blood vessels, all of which can severely impair vision.
- Retinitis Pigmentosa (RP): This is a group of inherited genetic disorders that cause the progressive breakdown and loss of photoreceptor cells. It typically begins with night blindness and loss of peripheral vision, eventually leading to tunnel vision and, in many cases, legal blindness.
Conventional treatments often focus on slowing disease progression, such as anti-VEGF injections for wet AMD, but they do not restore lost cells or reverse existing damage. This therapeutic gap is what makes the concept of regeneration so compelling.
An Introduction to Therapeutic Peptides
Peptides are naturally occurring biological molecules that consist of short chains of amino acids linked by peptide bonds. They are smaller than proteins and often act as highly specific signaling molecules, regulating a vast array of physiological processes, including inflammation, cell growth, and tissue repair.
Their therapeutic potential stems from several key characteristics:
- High Specificity: Peptides can be designed to bind to specific receptors, allowing for targeted effects with potentially fewer off-target side effects than small-molecule drugs.
- Biological Function: Many therapeutic peptides are derived from or mimic endogenous human proteins, leveraging the body’s own repair and regulatory pathways.
- Safety Profile: As they are composed of amino acids, peptides typically break down into non-toxic components, which can contribute to a favorable safety profile.
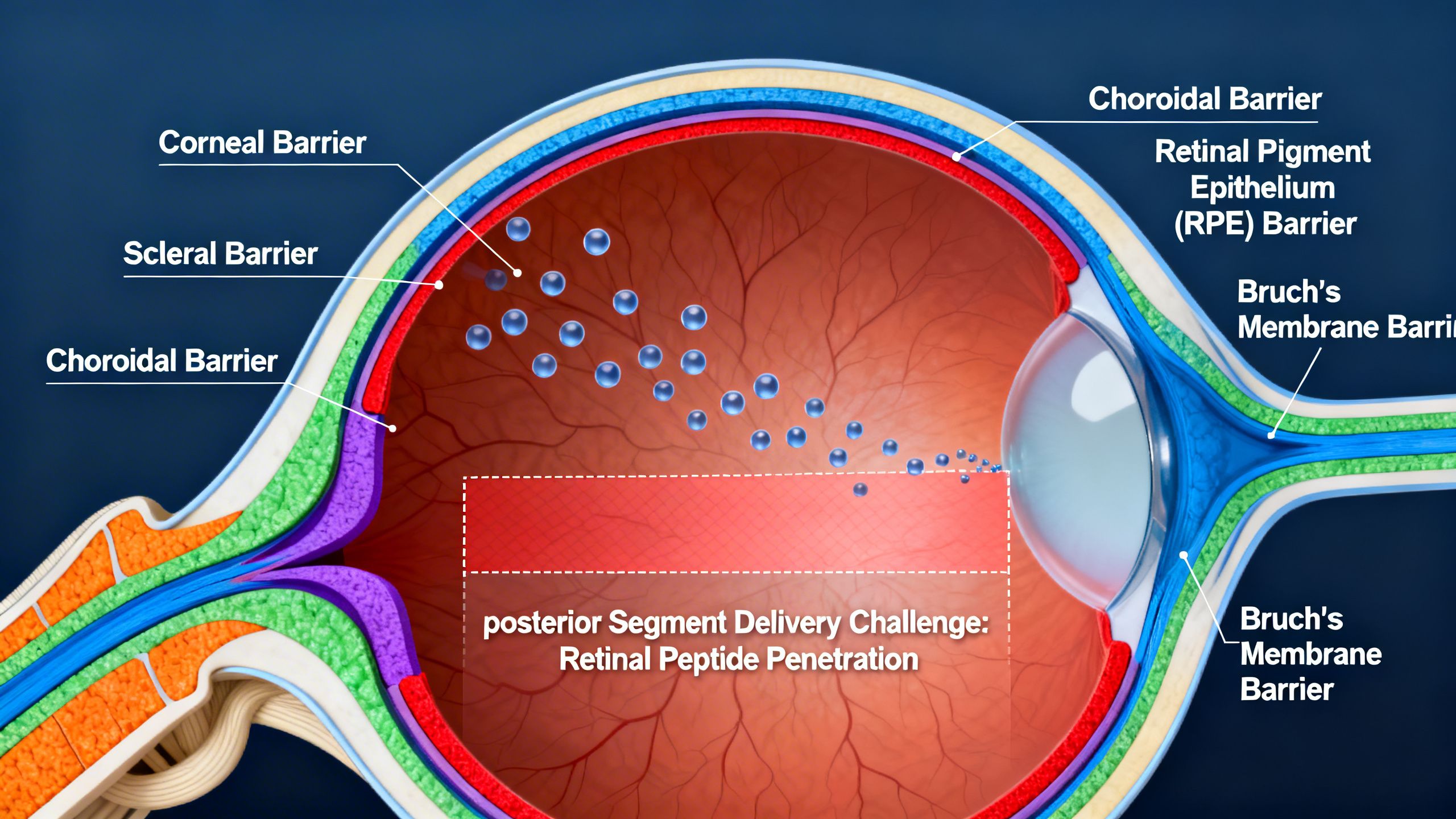
However, they also face significant challenges, primarily related to delivery and stability. Many peptides are quickly degraded by enzymes in the body and have difficulty crossing biological barriers, such as the blood-retina barrier, to reach their target tissue. Researchers are actively developing novel delivery systems, such as nanoparticles, hydrogels, and intravitreal implants, to overcome these hurdles.
Investigating Specific Peptides for Eye Regeneration
A number of peptides, many sold as unregulated “research chemicals,” have gained popularity for their purported regenerative effects. It is crucial to separate anecdotal claims from scientific evidence, particularly human clinical data. Below, we examine several compounds often discussed in the context of peptides for eye regeneration.
Thymosin Beta-4 (TB-4)
Thymosin Beta-4 is a naturally occurring peptide found in virtually all human cells, with particularly high concentrations in platelets and white blood cells. It is a primary regulator of actin, a protein essential for cell structure and movement. Its regenerative potential is linked to its ability to promote cell migration, reduce inflammation, inhibit apoptosis (programmed cell death), and stimulate the formation of new blood vessels.
Evidence in Eye Health:
TB-4 has been most extensively studied for its role in corneal wound healing. Human studies have investigated a sterile, preservative-free eye drop formulation of TB-4 for treating neurotrophic keratitis, a rare degenerative disease of the cornea. The research showed that TB-4 could promote healing of the corneal surface.
Regarding the retina, the evidence is currently limited to preclinical animal models. In studies of retinal injury and diseases like diabetic retinopathy, TB-4 has been shown to have neuroprotective effects, preserving retinal neurons from damage. It may also modulate the inflammatory response that contributes to retinal degeneration. However, there are no robust human clinical trials demonstrating that TB-4 can regenerate retinal cells or restore vision in patients with AMD or retinitis pigmentosa. The primary challenge remains delivering the peptide effectively to the back of the eye.
BPC-157
Body Protection Compound 157 (BPC-157) is a synthetic peptide derived from a protein found in human gastric juice. It has garnered significant attention for its potent, systemic healing capabilities observed in animal studies across a wide range of tissues, including muscle, tendon, bone, and the nervous system. Its proposed mechanisms include promoting angiogenesis (the formation of new blood vessels), modulating growth factors, and exerting strong anti-inflammatory effects.
Evidence in Eye Health:
Research on BPC-157 for eye conditions is still in its infancy and is confined to animal models. Studies have explored its use in healing corneal abrasions and chemical burns in rats, where it appeared to accelerate repair. Some animal research has also suggested it may counteract increases in intraocular pressure, a key factor in glaucoma.
Crucially, there is no published human research on the use of BPC-157 for any retinal condition, including AMD or diabetic retinopathy. Claims about its ability to reverse retinal damage are purely speculative and not supported by clinical evidence. Furthermore, its pro-angiogenic properties could be a double-edged sword; while promoting blood vessel growth is beneficial for healing some tissues, it could be detrimental in conditions like wet AMD and proliferative diabetic retinopathy, where abnormal blood vessel growth is the primary driver of vision loss. This makes its theoretical application in certain retinal diseases highly problematic and potentially dangerous.

GHK-Cu (Copper Peptide)
GHK-Cu is a naturally occurring copper-peptide complex found in human plasma, saliva, and urine. Its levels decline with age. GHK-Cu is known for its wound healing, anti-inflammatory, and antioxidant properties. It stimulates the synthesis of collagen and other key components of the extracellular matrix, and it has been shown to modulate the expression of numerous genes related to tissue repair and remodeling.
Evidence in Eye Health:
Most of the commercial application of GHK-Cu is in cosmetics for skin rejuvenation. Its connection to retinal health is largely theoretical, based on its general regenerative properties. It is hypothesized that its antioxidant and anti-inflammatory effects could help protect retinal cells from oxidative stress, a key contributor to the development of dry AMD.
Some in-vitro studies suggest GHK-Cu can promote the survival of certain neuronal cells. However, similar to BPC-157, there is a complete lack of human clinical trials investigating GHK-Cu for retinal regeneration or the treatment of any retinal disease. The challenge of delivering it to the retina in sufficient concentrations remains a major barrier. Any discussion of its use for eye health is speculative and extrapolates from its known effects on other tissues like skin.
Epitalon
Epitalon is a synthetic tetrapeptide (a peptide composed of four amino acids) that was developed in Russia. It is purported to be a synthetic version of a peptide extract from the pineal gland called Epithalamin. Proponents claim it functions as a telomerase activator, helping to lengthen telomeres—the protective caps at the ends of chromosomes that shorten with cell division and age. By extending telomere length, it is theorized to combat cellular aging.
Evidence in Eye Health:
Several small-scale Russian studies from the early 2000s reported that Epithalamin (the pineal extract) had beneficial effects in patients with degenerative retinal diseases, including retinitis pigmentosa. The studies claimed that treatment led to a widening of the visual field and improved visual acuity in a subset of patients.
However, these studies have significant limitations. They were often small, lacked rigorous control groups, and have not been replicated by independent researchers outside of Russia. The methodology and data reporting do not meet modern clinical trial standards. There are no high-quality, randomized, controlled trials published in major international journals to validate these claims for either Epithalamin or the synthetic Epitalon. As such, its efficacy as an AMD therapy peptide or for any other retinal condition remains unproven and highly questionable.
Peptides Derived from Endogenous Growth Factors
While the aforementioned peptides are popular in biohacking communities, the most promising research into retinal peptides is focused on developing drugs from naturally occurring neurotrophic and anti-angiogenic factors found within the eye itself. This approach is more targeted and biologically plausible.
Ciliary Neurotrophic Factor (CNTF)-Derived Peptides
CNTF is a powerful protein that promotes the survival of neurons, including retinal photoreceptors. Clinical trials using an encapsulated cell technology to deliver CNTF directly into the eye have shown it can slow the loss of photoreceptors in patients with retinitis pigmentosa and geographic atrophy (the advanced form of dry AMD). However, treatment with the full CNTF protein can cause side effects, such as weight loss and pupil constriction, and its large size makes delivery complex.
To address this, researchers are developing smaller peptides derived from the active sites of the CNTF protein. The goal is to create a molecule that retains the neuroprotective benefits of CNTF while having a better safety profile and improved ability to penetrate retinal tissue. This research is still in the preclinical stage but represents a more scientifically grounded approach to developing a peptide-based therapy.
Pigment Epithelium-Derived Factor (PEDF)-Derived Peptides
PEDF is one of the most potent natural inhibitors of angiogenesis in the eye. It also has strong neuroprotective and anti-inflammatory properties. In wet AMD and diabetic retinopathy, the balance between pro-angiogenic factors (like VEGF) and anti-angiogenic factors (like PEDF) is disrupted, leading to abnormal blood vessel growth.
Anti-VEGF injections are the current standard of care, but they require frequent administration and some patients become non-responsive. Peptides derived from PEDF are being investigated as an alternative or complementary therapy. A 44-amino acid peptide fragment of PEDF, for example, has been shown in animal models to be as effective as the full-length protein at inhibiting abnormal blood vessel growth and protecting retinal cells. Human clinical trials have been initiated to test the safety and efficacy of such peptides, representing a direct and promising application of AMD therapy peptides.
Mechanisms, Safety, and Unanswered Questions
The overarching hypothesis for how retinal peptides might work involves a multi-pronged approach:
- Neuroprotection: Shielding vulnerable retinal cells (photoreceptors, RPE cells, ganglion cells) from stress, toxins, and inflammatory damage.
- Anti-Inflammation: Modulating the chronic inflammatory response that drives the progression of diseases like AMD and diabetic retinopathy.
- Anti-Angiogenesis: Inhibiting the growth of leaky, abnormal blood vessels, a hallmark of wet AMD and proliferative diabetic retinopathy.
- Cellular Regeneration: Stimulating the body’s own repair mechanisms, though true regeneration of complex neural tissue like the retina remains a monumental challenge.
Safety and Regulation:
It is critical to underscore the safety concerns. Peptides like BPC-157, GHK-Cu, and Epitalon are not approved by the FDA or any other major regulatory agency for medical use. They are sold online as “research chemicals not for human consumption.” This means there is no oversight of their manufacturing, purity, or sterility. Contaminants or incorrect dosages could lead to serious harm, including infection or unpredictable biological effects. Self-administering these compounds, especially via injection, carries significant health risks.
Human Evidence for Peptides in Retinal Disease: What We Know So Far
At present, direct human evidence supporting peptide-based retinal regeneration is extremely limited. Most compounds commonly discussed in peptide research—such as TB-4, BPC-157, GHK-Cu, or Epitalon—have not been evaluated in controlled human trials for retinal degenerative diseases, and none are approved for ophthalmic use.
The most relevant human research in this area involves larger endogenous proteins or biologically derived factors, or experimental delivery systems designed to support retinal cell survival rather than regenerate lost tissue. These studies provide important mechanistic insight, but they should not be interpreted as proof of retinal regeneration or vision restoration.
Ciliary Neurotrophic Factor (CNTF)
Ciliary Neurotrophic Factor is a naturally occurring protein with well-documented neuroprotective effects on retinal photoreceptors. In human clinical research, CNTF has been investigated using encapsulated cell technology, an implantable device that continuously releases CNTF into the vitreous cavity.
In multi-center randomized clinical trials involving patients with late-stage retinitis pigmentosa and geographic atrophy, CNTF delivery was associated with preservation of retinal structure, as measured by photoreceptor outer segment area on retinal imaging over a two-year period. Importantly, these studies did not demonstrate improvements in visual acuity or visual function.
These findings suggest that CNTF may slow certain structural aspects of retinal degeneration, but they do not indicate retinal regeneration or functional recovery. Additionally, CNTF is a large protein rather than a short peptide, and its delivery requires specialized implants, limiting direct relevance to commonly discussed research peptides.
Pigment Epithelium-Derived Factor (PEDF) and Peptide Fragments
Pigment Epithelium-Derived Factor is an endogenous protein with strong anti-angiogenic, neuroprotective, and anti-inflammatory properties in the retina. It plays a key role in maintaining the balance between pro-angiogenic and anti-angiogenic signaling in the eye, a process that is disrupted in conditions such as wet age-related macular degeneration and diabetic retinopathy.
Research has identified shorter peptide fragments derived from PEDF that retain some of these biological activities. In animal models and laboratory studies, PEDF-derived peptides have been shown to inhibit abnormal blood vessel growth and protect retinal cells from stress-induced damage.
Human data on PEDF-derived peptides remain very limited and preliminary. Early-phase investigations have primarily focused on safety and biological plausibility rather than clinical efficacy, and results from small or exploratory studies cannot be used to draw conclusions about therapeutic benefit. Larger, controlled trials would be required to determine whether PEDF-based peptides offer meaningful advantages over existing anti-VEGF therapies.
Thymosin Beta-4 (TB-4) and Ocular Surface Research
Thymosin Beta-4 is a naturally occurring peptide involved in cell migration, inflammation regulation, and tissue repair. Its most robust human evidence in ophthalmology relates to corneal healing, not retinal disease.
A Phase III randomized, controlled clinical trial evaluated a topical formulation of Thymosin Beta-4 (RGN-259) for the treatment of neurotrophic keratopathy, a degenerative condition affecting the corneal surface. The study found that patients receiving the peptide eye drops were more likely to achieve complete corneal epithelial healing compared to placebo.
While these findings demonstrate regenerative activity in ocular surface tissue, they cannot be extrapolated to the retina. The cornea and retina differ substantially in structure, function, and biological accessibility, and Thymosin Beta-4 has not been shown in human studies to regenerate retinal tissue or restore vision in retinal degenerative diseases.
Interpreting the Evidence Responsibly
Taken together, existing human research supports the concept of neuroprotection and disease modulation, rather than true retinal regeneration. Even in the most advanced studies, observed benefits are typically structural or biochemical and do not translate into restored visual function.
For commonly discussed research peptides such as BPC-157, GHK-Cu, Epitalon, and similar compounds, evidence remains limited to animal models, in-vitro studies, or theoretical mechanisms. None have demonstrated clinical efficacy in human retinal disease, and none are approved for ophthalmic use.
As research progresses, peptide-based therapies may eventually play a role in supporting retinal health or slowing degeneration. However, current evidence does not support claims of retinal regeneration or vision restoration from peptide therapies, and such claims should be viewed with caution until validated by well-designed human clinical trials.
Conclusion: Promise Tempered by Caution
The concept of using retinal peptides to combat vision loss is undeniably exciting and represents a frontier in ophthalmology. The potential to protect neurons, reduce inflammation, and halt abnormal blood vessel growth offers a multi-faceted approach that could complement or even surpass current treatments. Scientifically grounded research into peptides derived from endogenous factors like CNTF and PEDF is already progressing into human trials, marking a significant step toward translating this promise into a clinical reality.
However, it is imperative to maintain a clear-eyed perspective. The hype surrounding unregulated research peptides like BPC-157 and Epitalon has far outpaced the scientific evidence. For these compounds, there is a profound lack of human data for retinal conditions, and their safety profiles are unknown. The theoretical benefits are often overshadowed by practical challenges of delivery and potential for harm, especially with pro-angiogenic peptides in the context of AMD.
As research continues, the future may hold targeted, approved peptide therapies for a range of retinal diseases. Until then, patients must rely on evidence-based, approved treatments and view the claims surrounding experimental peptides for eye regeneration with extreme caution, always consulting with a qualified medical professional before considering any unproven therapy.
References and Further Reading
1. PEDF-derived neuroprotective peptides for retinal degeneration
This research shows short peptides derived from PEDF (Pigment Epithelium Derived Factor) can reach the retina and protect photoreceptors in models of retinitis pigmentosa and AMD, slowing degeneration.
https://www.nature.com/articles/s43856-025-00789-8
2. NIH news on PEDF peptide eye drops slowing vision loss
NIH press release covering the same PEDF-derived peptide eye drops that showed slowed photoreceptor degeneration in animal models, supporting the scientific direction.
https://www.nih.gov/news-events/nih-research-matters/peptide-eye-drops-may-help-protect-vision
3. Anti-angiogenic PEDF-derived peptides
This paper shows smaller PEDF peptides exhibit anti-VEGF and anti-angiogenic effects, useful in treating neovascular retinal diseases.
https://link.springer.com/article/10.1186/s12886-022-02295-0
4. PEDF peptides mitigate abnormal vessel growth (animal models)
This research identifies PEDF-derived fragments that reduce choroidal neovascularization (CNV), a model for wet AMD.
https://pubmed.ncbi.nlm.nih.gov/31520600/
5. PEDF-derived peptide inhibits retinal angiogenesis
A classic peer-reviewed study showing synthetic PEDF peptide fragments suppress VEGF and pathologic blood vessel growth in animal eye models.
https://pubmed.ncbi.nlm.nih.gov/22386653/
6. Overview of GHK-Cu gene modulation and regenerative biology
While not retina-specific, this review is one of the highest-quality peer-reviewed human studies on GHK-Cu’s gene regulatory and repair properties, relevant background.
https://pubmed.ncbi.nlm.nih.gov/29986520/