Inflammation is a vital biological process that protects the body from infection and injury. However, mounting evidence suggests that chronic inflammation plays a central role in the aging process and the development of many degenerative diseases. Understanding the link between inflammation and aging—often referred to as “inflammaging”—is critical for developing strategies to promote healthier, longer lives. This article reviews the latest human research, explains key mechanisms, and highlights potential interventions targeting inflammation aging, including emerging compounds such as BPC-157 and omega-3 fatty acids.

What Is Inflammation and Why Does It Matter in Aging?
Inflammation is the body’s natural response to harmful stimuli, such as pathogens, damaged cells, or irritants. Acute (short-term) inflammation is typically beneficial, enabling tissue repair and fighting infection. In contrast, chronic (long-term) inflammation becomes persistent and can disrupt normal cell function, ultimately driving tissue damage and disease progression.
Key Points:
- Chronic inflammation becomes more common with age—a phenomenon called inflammaging.
- This persistent, low-grade inflammation is rarely symptomatic but can promote cell damage across various organs.
- Inflammaging is linked to a heightened risk of multiple age-related diseases, including cardiovascular disease, neurodegeneration, metabolic syndrome, and osteoporosis.
Mechanisms Connecting Inflammation & Aging
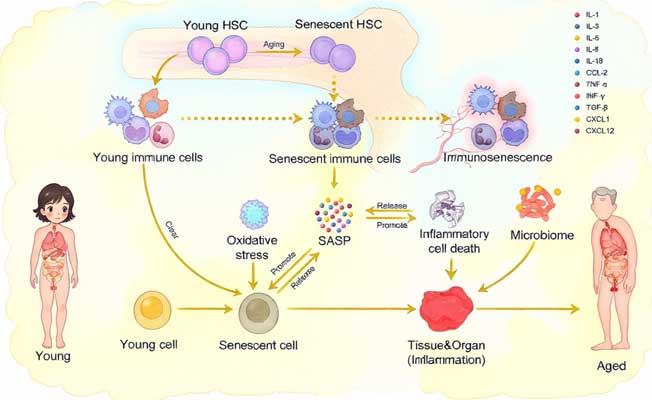
1. Immune System Dysfunction
With age, the immune system undergoes significant changes—both its ability to mount defenses (immunosenescence) and increased production of pro-inflammatory signals. This imbalance can:
- Diminish pathogen defense
- Increase autoimmunity
- Promote chronic inflammation even in the absence of infection
2. Cellular Senescence
Senescent cells are older, damaged cells that have lost the ability to divide. Rather than dying, they remain in tissue and secrete pro-inflammatory molecules (the senescence-associated secretory phenotype, or SASP), fueling a cycle of local inflammation that can damage neighboring cells.
3. Mitochondrial Dysfunction and Oxidative Stress
As we age, mitochondrial efficiency declines, leading to more oxidative stress and molecular byproducts that trigger an inflammatory response. This creates a feedback loop, exacerbating both mitochondrial dysfunction and inflammation.
4. Gut Microbiome Imbalance
The composition of the gut microbiota changes with age. Increased permeability (sometimes called “leaky gut”) can enable bacterial products to enter the bloodstream, activating chronic inflammation in distant organs.
Chronic Inflammation and Degenerative Diseases
Many of the world’s most prevalent diseases of aging share an inflammatory basis. Here are key examples:
Cardiovascular Disease
Atherosclerosis—the thickening and hardening of arteries—is driven largely by inflammation in the arterial walls. Disrupted immune signaling and persistent pro-inflammatory molecules play a pivotal role in plaque development and instability.
Neurodegeneration
Alzheimer’s and Parkinson’s diseases feature chronic inflammation in the brain. Microglia (the brain’s immune cells) can become persistently activated, releasing cytokines that damage neurons and contribute to cognitive decline. For more detail, see Neurodegeneration in Aging.
Metabolic Syndrome and Type 2 Diabetes
Adipose (fat) tissue, especially when in excess, often becomes inflamed and secretes inflammatory cytokines. This process impairs insulin sensitivity, further fueling metabolic syndrome and diabetes.
Osteoporosis
Inflammatory cytokines such as TNF-α and IL-6 disrupt the balance between bone formation and resorption, accelerating bone loss with age.
Causes of Chronic Inflammation in Aging
Several factors drive chronic inflammation as we age:
- Adiposity: Accumulation of visceral fat increases pro-inflammatory cytokine production.
- Physical Inactivity: Sedentary lifestyles are associated with higher baseline inflammation.
- Nutritional Deficiencies: Diets low in anti-inflammatory nutrients (e.g., omega-3 fatty acids) and antioxidants can worsen chronic inflammation aging.
- Persistent Viral Infections: Latent viruses (such as CMV or HSV) can chronically activate the immune system.
- Environmental Toxins: Pollution, smoke, and alcohol contribute to a systemic pro-inflammatory state.
Diagnosing and Measurement
Although precise diagnosis is challenging, common biomarkers of inflammation used in clinical and research settings include:
- C-reactive protein (CRP, especially high-sensitivity CRP)
- Interleukin-6 (IL-6)
- Tumor necrosis factor alpha (TNF-α)
- White blood cell count
Notably, these markers become less specific with age due to other comorbidities. Regular health screenings and viewing trends over time remain key.
Strategies to Manage Inflammation in Aging
1. Lifestyle Interventions
Exercise
- Both aerobic and resistance training can lower CRP and improve immune function.
Diet
- Mediterranean-style diets rich in fruits, vegetables, legumes, and omega-3 fatty acids reduce inflammatory biomarkers.
- Limiting ultra-processed foods, sugar, and saturated fats is crucial.
Body Weight
- Maintaining a healthy weight, particularly reducing visceral adiposity, consistently reduces systemic inflammation.
2. Pharmaceutical Therapies
- Aspirin, NSAIDs: Widely used but not suitable for chronic prevention due to side effects.
- Statins: Besides lowering cholesterol, statins have anti-inflammatory effects.
- Metformin: Used in diabetes, metformin has shown anti-inflammatory activity in older adults.
3. Targeted Compounds & Supplements: Human Evidence
Omega-3 Fatty Acids
Omega-3s (particularly EPA and DHA from fish oil) have been shown to reduce systemic inflammation and help prevent cardiovascular disease.
BPC-157: A Peptide in Focus
BPC-157 is a synthetic peptide gaining attention for its anti-inflammatory and tissue-repair-promoting effects. Early human trials suggest:
- Acceleration of wound healing
- Improved gut barrier integrity
- Reduced inflammatory pain
Its long-term safety and efficacy in broader aging populations, however, require further research.

Additional Interventions
- Curcumin (from turmeric): May modestly lower certain inflammatory markers.
- Vitamin D: Deficiency is associated with increased inflammation; supplementation lowers risk in some older adults.
- Probiotics/Prebiotics: Can rebalance the gut microbiome to reduce local and systemic inflammation.
Note: Always consult a healthcare provider before starting any supplement, especially in the presence of chronic conditions or when taking multiple medications.
Peptides and Emerging Therapies in Inflammaging
There is growing interest in peptides for inflammation due to their potential to modulate immune responses and facilitate tissue repair. Besides BPC-157, other peptides are under investigation, but large-scale, long-term human data are lacking.
Key considerations:
- Individual responses can vary greatly
- Regulatory oversight of peptide-based supplements is inconsistent
- Most evidence is still preliminary

Individual Variability: Why Inflammation Affects People Differently
Not all older adults experience the same degree of chronic inflammation or risk for degenerative diseases. Factors that modify individual risk include:
- Genetic predispositions (e.g., polymorphisms influencing cytokine production)
- Lifetime history of infections and immune challenges
- Diet, physical activity, and environmental exposures
- Microbiome composition
Understanding these variables may eventually enable more personalized interventions in healthy aging.
Future Directions & Ongoing Research
Scientists are now:
- Testing anti-inflammatory biologics used in autoimmune disease for aging-related conditions
- Investigating how intermittent fasting and caloric restriction impact inflammaging
- Researching senolytics (compounds that clear senescent cells) as a way to reduce SASP-driven inflammation
Large, long-term clinical trials are needed to clarify who will benefit most, optimal intervention timing, and combined approaches to maximizing healthspan.
Key Takeaways
- Chronic, low-level inflammation is a hallmark of aging and a major driver of degenerative disease risk.
- Strategies with the strongest evidence include regular exercise, a Mediterranean-style diet, omega-3 supplementation, and maintaining a healthy weight.
- Emerging interventions like BPC-157 and other peptides show potential but require more robust, high-quality human evidence.
- Monitoring inflammatory markers and personalizing approaches based on risk factors are important steps for individuals and clinicians.
- Interventions targeting chronic inflammation aging may significantly extend healthy years of life and reduce disease burden.
Studies / References
1. A systematic review and meta-analysis found that aerobic exercise training in older adults significantly lowers inflammatory biomarkers including CRP, IL-6, and TNF-α, demonstrating the anti-inflammatory effects of regular physical activity with aging. https://link.springer.com/article/10.1186/s13102-025-01279-z
2. Observational human research suggests increased intake of anti-inflammatory diet components, such as fruits, vegetables, and healthy fats, along with physical activity, is associated with lower systemic inflammatory markers in elderly adults, indicating a potential strategy to counteract inflammaging. https://pubmed.ncbi.nlm.nih.gov/34835952/
3. In an RCT involving older adults, an omega-3 enriched high-protein diet combined with exercise reduced circulating pro-inflammatory markers and affected inflammatory gene expression in immune cells, highlighting dietary modulation of inflammaging. https://pubmed.ncbi.nlm.nih.gov/36674453/
4. A meta-analysis of observational studies showed that adherence to a Mediterranean dietary pattern is significantly associated with lower levels of CRP and other inflammatory indicators in older individuals, supporting the diet’s anti-inflammatory role. https://pubmed.ncbi.nlm.nih.gov/33002104/
5. A narrative review of nutritional interventions in aging found that healthy diets including Mediterranean-style patterns, balanced gut microbiota, and calorie restriction are linked to reduced systemic inflammation and improved immune function in the elderly. https://pubmed.ncbi.nlm.nih.gov/35219904/
Disclaimer: This content is for educational purposes and should not replace personalized clinical advice. Always consult a healthcare provider before making decisions about managing inflammation aging or starting new therapies.