Raloxifene has emerged as a significant selective estrogen receptor modulator (SERM) in the field of musculoskeletal health, especially for aging populations. As both the understanding and treatment of age-related degeneration advance, its role in supporting bone and muscle integrity is gaining attention. This article provides an expert overview of how raloxifene works, what the evidence says about its benefits and risks, and practical considerations for its use in older adults.
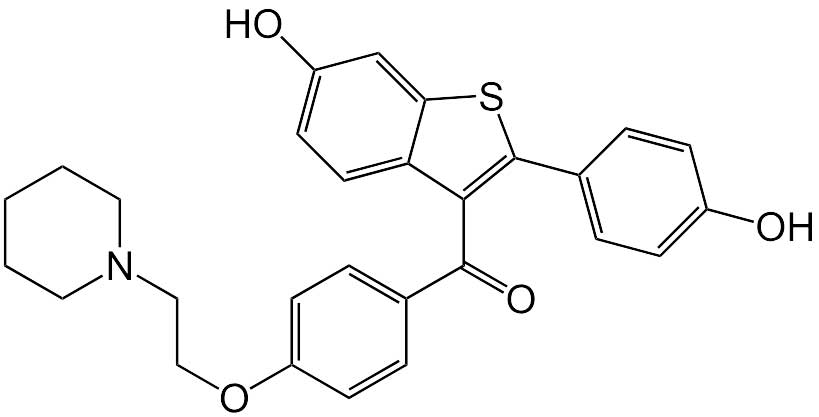
Understanding Raloxifene and SERMs
Selective estrogen receptor modulators (SERMs) are compounds that interact with estrogen receptors differently in various tissues. Raloxifene acts as an estrogen agonist in bone while behaving as an antagonist in breast and uterine tissue. This tissue-selective action makes SERMs like raloxifene uniquely suited for addressing conditions like osteoporosis without the risks associated with conventional hormone replacement therapy.
Key properties of raloxifene:
- Mimics estrogen effects on bone, reducing bone loss
- Blocks estrogen receptors in breast and uterus, lowering cancer risk
- Does not stimulate endometrial growth
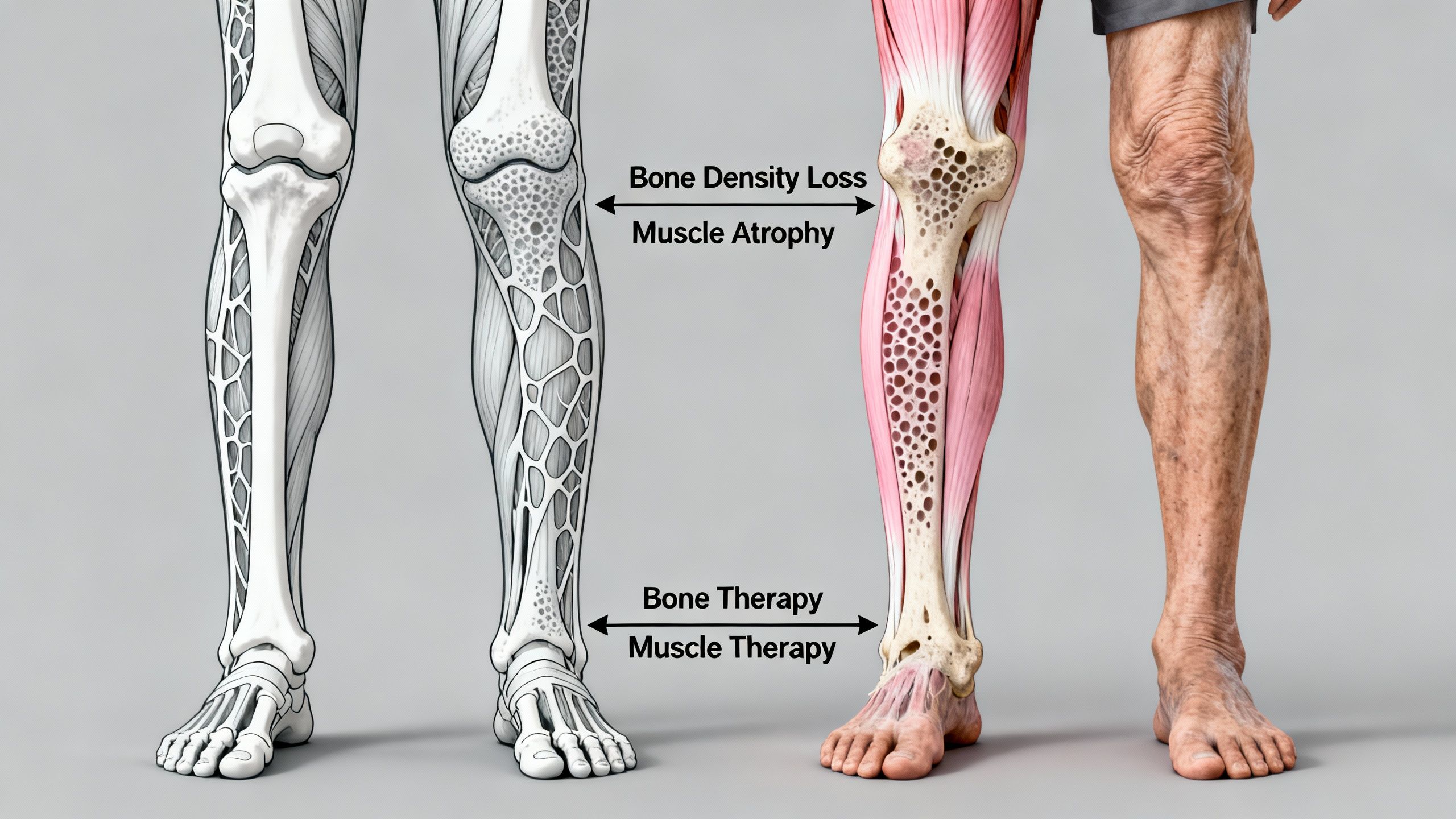
Why Focus on Bone and Muscle in Aging?
With advancing age, both men and women experience:
- Decreased bone density (osteopenia/osteoporosis), leading to fractures
- Loss of muscle mass and function (sarcopenia), affecting mobility and independence
Interventions targeting both bone and muscle are central to healthy aging, reducing falls, fractures, and disability.
How Raloxifene Works: Mechanisms of Action
Effects on Bone
Raloxifene binds to estrogen receptors in bone, promoting gene transcription patterns that limit bone resorption (breakdown). This helps maintain or increase bone mineral density, especially in the spine and hip. Unlike full estrogen, it does not increase risk for certain cancers.
Effects on Muscle
While raloxifene was developed primarily for bone health, some early human studies suggest potential muscle benefits. These effects—such as modest preservation of lean mass or improved physical function—remain exploratory and are not an approved indication. Current evidence is limited to small trials or secondary analyses, and more research is needed before definitive recommendations can be made. Its action in muscle tissue is less direct and possibly related to:
- Modulation of local estrogen signaling
- Reduction of inflammation
- Potential positive effects on muscle quality and fat infiltration
Biological Pathways
- Osteoblast and osteoclast regulation: Raloxifene inhibits osteoclasts (cells that break down bone) while supporting osteoblast function (cells that build bone).
- Collagen and extracellular matrix: Some evidence hints at beneficial effects on collagen synthesis in both bone and muscle.
- Inflammatory cytokines: By modulating inflammatory processes, it could indirectly support muscle function in aging.
Human Evidence: Clinical Outcomes
The majority of raloxifene’s data comes from studies in postmenopausal women with osteoporosis. However, emerging trials are now investigating its muscle effects, particularly in the context of aging.
Bone Health Benefits
- Increases or maintains bone mineral density in the lumbar spine and femoral neck
- Reduces risk of vertebral fractures (but not necessarily hip fractures)
Muscle Health Investigations
While evidence is more limited, some human studies show:
- Preservation of lean mass in postmenopausal women compared to placebo
- Potential reduction in falls and improvement of physical function, though findings are inconsistent
Important: The effectiveness of raloxifene for muscle preservation is not as robust as for bone. More research is needed, especially in men and in those with advanced muscle loss.
Raloxifene Use in Clinical Practice
Who Might Benefit?
- Postmenopausal women with osteoporosis or high fracture risk
- Women intolerant of standard hormone therapy due to cancer risk
- Individuals with early sarcopenia (potential but experimental)
Dosage and Administration
- Standard dose: 60 mg tablet, once daily (oral)
- Taken with or without food
Duration of Therapy
- Benefits continue with ongoing use, but individual risk profiles should be periodically reassessed by a healthcare professional
Raloxifene Muscle and Bone Therapy: Practical Considerations
Advantages
- Proven to reduce vertebral fracture risk
- Favorable safety profile for breast and uterine tissue
- Oral, easy to administer
Limitations
- No reduction in hip fracture risk
- Not approved for muscle loss or sarcopenia
- Data in men and diverse populations are scarce
Safety and Side Effects
| Common Side Effects | Rarer but Serious Risks |
|---|---|
| Hot flashes | Venous thromboembolism (VTE) |
| Leg cramps | Stroke (in higher-risk older women) |
| Peripheral edema | Fatal stroke (women with CHD risk) |
| Flu-like symptoms |
Caution: Raloxifene increases the risk of blood clots. It should be avoided in anyone with a history of venous thromboembolism, stroke, or severe cardiovascular risk factors.
Real-World Use and Individual Variability
- Response to raloxifene varies by age, baseline bone/muscle health, and genetic background
- Some respond with significant gains in bone mineral density; others see minimal effect
- Muscle effects, if any, are generally modest
Monitoring and Follow-Up
- Bone density scans (DXA) every 1–2 years
- Blood clot risk assessment at baseline and during therapy
Comparisons to Other Bone and Muscle Therapies
| Therapy Type | Bone Benefit | Muscle Benefit | Safety Profile |
|---|---|---|---|
| Raloxifene | Moderate | Possibly mild | Moderate (VTE risk) |
| Bisphosphonates | Strong | None | Good, except renal/hear |
| Denosumab | Strong | None | Good, rare hypocalcemia |
| HRT (estrogen) | Strong | Possible | Poor (cancer, CV risk) |
| SARMs (selective androgens) | Not approved | Research only | Unclear (not approved) |
Incorporating Raloxifene Into Healthy Aging Strategies
While not a substitute for healthy lifestyle intervention, raloxifene can be part of a comprehensive plan:
- Lifestyle First: Encourage weight-bearing exercise, protein-rich diet, and vitamin D adequacy.
- Bone-Protective Agents: Consider raloxifene if bisphosphonates are unsuitable.
- Regular Monitoring: Assess bone, muscle strength, and cardiovascular risk regularly.

Potential Interactions and Special Precautions
- Avoid concurrent use with other estrogens or tamoxifen
- Caution with cholesterol-lowering medications, as raloxifene may have modest lipid effects
- Renal impairment: Use with care
- Not recommended during immobilization (e.g., after surgery) due to clot risk
Gender Differences and Raloxifene
While the vast majority of research is in postmenopausal women, early pilot studies and theoretical frameworks suggest potential, albeit unproven, applications in:
- Older men with low bone density who cannot tolerate bisphosphonates
- Men with androgen deprivation therapy for prostate cancer (preventing osteoporosis)
Much more research is needed before routine use in men.
Future Research Directions
- Direct head-to-head trials against other osteoporosis drugs in diverse populations
- More robust studies on muscle mass and function in older adults (both genders)
- Long-term safety in those with multimorbidity (multiple chronic diseases)
Summary and Conclusions
Raloxifene is a well-studied SERM with a proven role in maintaining bone health and reducing spine fracture risk in postmenopausal women. While preclinical and early clinical studies offer hope for added benefit in muscle maintenance, these effects are still under active investigation and not yet an established indication. Individuals with osteoporosis, especially those at high risk for breast or uterine cancer, may benefit most from raloxifene therapy.
Cautions:
- Significant risk of blood clots; not for use in those with history of VTE
- No benefit in hip fracture reduction
- Effectiveness for muscle loss is unproven
For bone and muscle therapy in aging, it may be a valuable part of a larger clinical strategy focused on individualized risk-benefit assessment and lifestyle optimization.
Studies / References
- Raloxifene reduces vertebral fracture risk in postmenopausal osteoporosis — The Multiple Outcomes of Raloxifene Evaluation (MORE) Trial found that 60 mg daily significantly reduced new vertebral fracture risk compared with placebo over three years in postmenopausal women with osteoporosis. Vertebral fracture rates and increases in bone mineral density were seen, but non‑vertebral fracture effects were minimal.
https://pubmed.ncbi.nlm.nih.gov/12161484/ - Early clinical vertebral fracture reduction — Secondary analysis from the MORE trial showed a significant reduction in clinical vertebral fractures at 3–6 months in women treated with 60 mg/day raloxifene versus placebo, supporting early anti‑resorptive action on bone.
https://pubmed.ncbi.nlm.nih.gov/16368046/ - Effects on body composition and muscle strength — In a double‑blind, placebo‑controlled trial of postmenopausal women aged ≥ 70, raloxifene 60 mg/day significantly increased fat‑free mass (lean mass) compared with placebo over 12 months, but did not produce significant changes in muscle strength or power. This supports body composition changes but underscores that effects on functional muscle outcomes remain exploratory.
https://pubmed.ncbi.nlm.nih.gov/19884264/ - Safety profile: venous thromboembolism risk — Meta‑analysis of nine randomized trials (24,523 postmenopausal women) found that raloxifene therapy was associated with a significantly increased risk of deep venous thrombosis (DVT) and pulmonary embolism (PE) compared with non‑use, reinforcing clot risk as an important clinical consideration.
https://pubmed.ncbi.nlm.nih.gov/18278183/ - Pharmacovigilance and adverse event signals — A real‑world analysis of the FDA Adverse Event Reporting System identified thalromboembolic events, muscle spasms, and other adverse signals associated with raloxifene, highlighting the importance of ongoing surveillance and careful risk assessment in older adults.
https://pubmed.ncbi.nlm.nih.gov/39690869/
Key Takeaways
- Raloxifene reduces vertebral fracture risk and may help maintain bone density.
- Effects on muscle are unproven but under study.
- SERMs aging populations can benefit, especially when other therapies are unsuitable.
- Assess risks, especially for blood clots, before starting therapy.
- Long-term studies of bone and muscle therapy are essential to broaden use and confirm safety.



