Testosterone therapy is increasingly discussed as a potential strategy to combat age-related muscle loss, or sarcopenia. As adults age, declining hormone levels—particularly testosterone—are linked to decreased muscle mass and strength, impacting overall mobility and quality of life. This article provides a detailed, evidence-based overview of testosterone therapy: its mechanisms, benefits, risks, and practical considerations for aging adults focused on muscle health.
Understanding Testosterone and Muscle Health
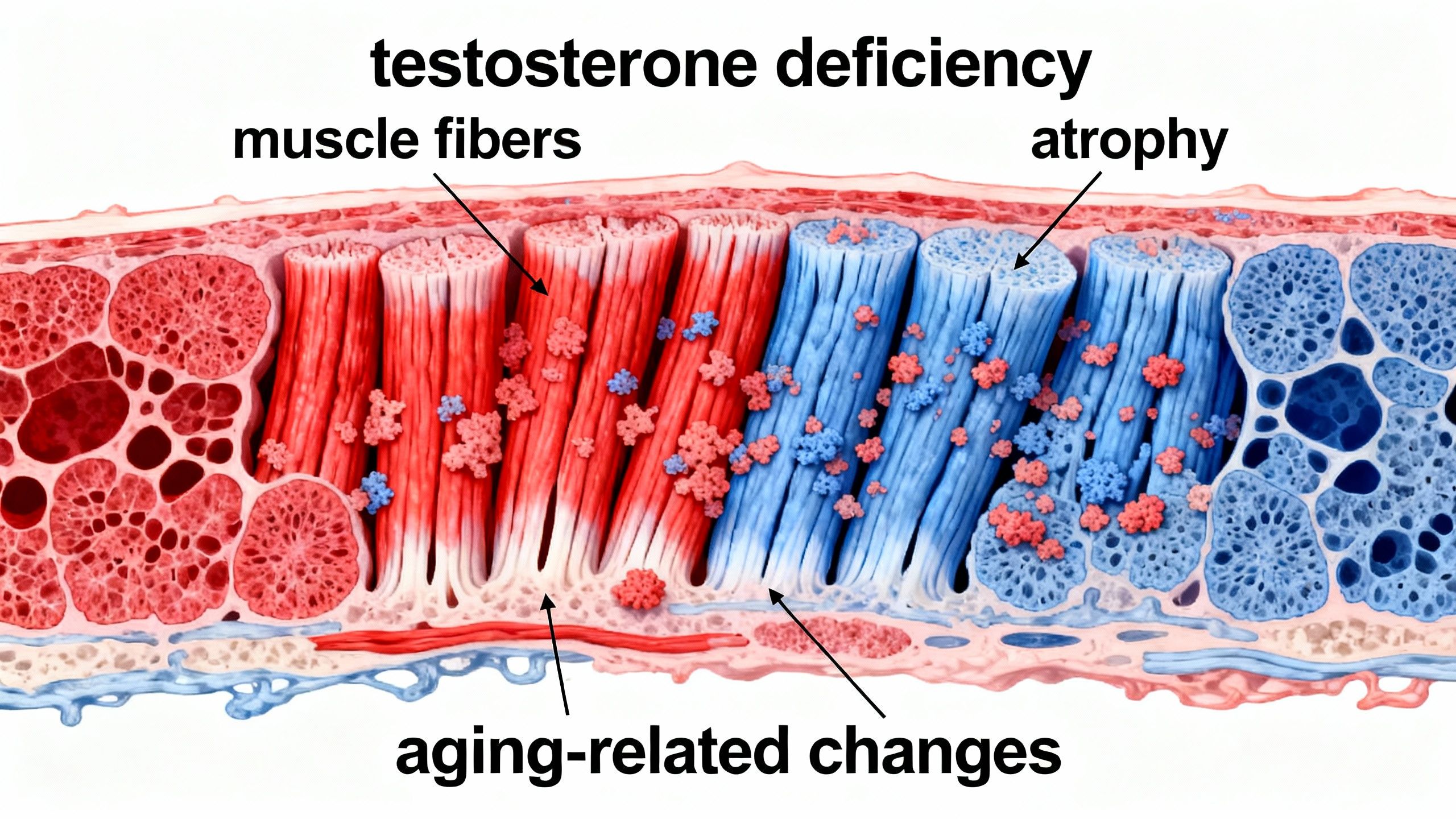
Testosterone is a key androgenic hormone responsible for the development and maintenance of male characteristics, muscle mass, bone density, and overall physical vitality. While men naturally experience a gradual decline in testosterone starting in their 30s, women also produce small amounts, and levels may fall post-menopause. Lower testosterone correlates with increased risks of frailty, sarcopenia, and impaired recovery from illness or injury, though causality varies by individual health status and activity level.
What Is Sarcopenia?
Sarcopenia refers to the loss of skeletal muscle mass and function that occurs with aging. It’s a major contributor to weakness, falls, loss of independence, and poor outcomes after hospitalization.
Key Factors Influencing Muscle Loss
- Hormonal changes: Decline in testosterone, growth hormone, estrogen.
- Physical inactivity: Reduced exercise levels with age.
- Nutritional deficits: Inadequate protein, vitamin D, or caloric intake.
- Chronic diseases: Diabetes, chronic inflammation, or organ dysfunction.
Mechanisms: How Testosterone Affects Muscle Health
Testosterone acts directly and indirectly on muscle tissue. It binds to androgen receptors in muscle cells, stimulating protein synthesis and muscle fiber growth, and may increase the activity of satellite cells involved in muscle repair.
- Enhances muscle protein synthesis by upregulating anabolic pathways (e.g., IGF-1).
- Reduces muscle breakdown via antagonism of catabolic hormones such as cortisol.
- Stimulates neuromuscular function: Improves nerve-muscle communication.
Testosterone therapy aging research shows these mechanisms are preserved—often blunted in advanced age or in chronic disease states—but the body’s response can be highly individual.
Clinical Benefits of Testosterone Therapy in Older Adults
1. Lean Muscle Mass (Most Consistent)
-
Testosterone therapy reliably increases lean body mass in men with low baseline testosterone.
-
Average gains: ~1–2 kg over 6–12 months.
-
These changes are biologically real but not always noticeable without strength training.
2. Muscle Strength (Variable)
-
Strength gains are inconsistent across trials.
-
Lower-body strength improves more reliably than upper-body strength.
-
Strength improvements are larger when therapy is combined with resistance exercise.
3. Physical Function (Most Clinically Meaningful, Least Predictable)
-
Measures such as walking speed, stair-climbing power, and fall risk show modest or no improvement in many trials.
-
Functional benefits tend to occur in:
-
Frail individuals
-
Those with very low baseline testosterone
-
Patients engaged in structured physical activity
-
Key Insight: Testosterone increases muscle mass more consistently than it improves strength, and improves function only in select populations.
| Outcome | Consistency of Benefit | Clinical Importance |
|---|---|---|
| Lean muscle mass | High | Moderate |
| Muscle strength | Moderate | High |
| Physical function | Low–Moderate | Very High |
Statistical Significance vs. Real-World Benefit
Many testosterone trials report statistically significant changes, meaning the results are unlikely due to chance. However, statistical significance does not always equate to clinical relevance.
In practice:
-
Gains in lean mass are often measurable but modest
-
Strength improvements are inconsistent
-
Functional outcomes (mobility, fall reduction) are the most meaningful but least consistently improved
This distinction is critical when counseling aging adults considering testosterone therapy.
Practical Applications: When Is Testosterone Therapy Used?
Who Might Benefit?
- Older men (usually over 60) with clinically proven low testosterone, notable muscle loss, or frailty.
- Select postmenopausal women with persistent muscle weakness unresponsive to other therapies (rare, and under research).
NOTE: Treatment must always be medically supervised, with careful assessment of risks and benefits.
Diagnostic Steps Before Considering Therapy
- Blood tests: Morning total and free testosterone on at least two occasions.
- Assessment of symptoms: Muscle loss, weakness, reduced mobility, fatigue, low libido.
- Screen for treatable conditions: Sleep apnea, anemia, thyroid dysfunction, or medication side effects.
Risks and Safety Considerations of Testosterone Therapy
Common Side Effects
- Mild fluid retention or weight gain
- Acne or oily skin
- Worsening of sleep apnea
- Mild breast tenderness or enlargement (men)
- Increased red blood cell count (may heighten clot risk)
Serious Risks and Caveats
Testosterone therapy may increase risks in certain populations:
- Prostate cancer: Although recent evidence suggests no major increase in risk with careful screening, those with a history of prostate or breast cancer should generally avoid therapy.
- Cardiovascular risk: Some studies show a small rise in heart attack or stroke, especially in older men with pre-existing heart conditions; newer research suggests neutral to modest risk when replacement is appropriately dosed and monitored in men with stable cardiovascular disease.
Testosterone therapy is not a general anti-aging cure or a replacement for exercise and nutrition.
Contraindications
- Diagnosed or suspected prostate or breast cancer
- Severely elevated red blood cell count (polycythemia)
- Untreated severe sleep apnea
- Uncontrolled heart failure
Individual Variability and Monitoring
- Responses vary dramatically. Some see marked improvement in muscle mass/strength, others little to no change.
- Regular monitoring (every 3–6 months) of hormone levels, blood counts, prostate health, and cardiovascular markers is essential.

Testosterone Therapy Regimens and Approaches
Approved Forms of Testosterone Therapy
| Form | Administration | Dosing Frequency | Notes |
|---|---|---|---|
| Gel/cream | Transdermal | Daily | Easiest to adjust, risk of skin transfer to others |
| Injection (IM or SC) | Intramuscular/subcutaneous | Every 1–4 weeks | Larger fluctuations in hormone levels |
| Patch | Transdermal | Daily | Skin irritation possible |
| Pellet implantation | Subcutaneous | Every 3–6 months | Minimally adjustable, risk of infection |
Oral testosterone forms are generally not recommended due to increased liver risk.
Adjunct Lifestyle and Medical Measures
Testosterone therapy works best alongside:
- Progressive resistance exercise (key for maximizing muscle gains)
- Adequate protein and nutrient intake
- Addressing underlying chronic diseases (e.g., diabetes, inflammation)
Testosterone Therapy in Women: Limited Evidence and Caution
While testosterone therapy is sometimes discussed for postmenopausal women with severe sarcopenia, evidence remains limited. Benefits for muscle mass are modest at best, and long-term safety profiles are less understood, with potential for masculinizing side effects.
- Use is not approved for general muscle maintenance in women.
- Always consult a specialist and consider alternative options first.
Resistance training and adequate protein intake remain the most evidence-supported interventions for preserving muscle health in aging women.
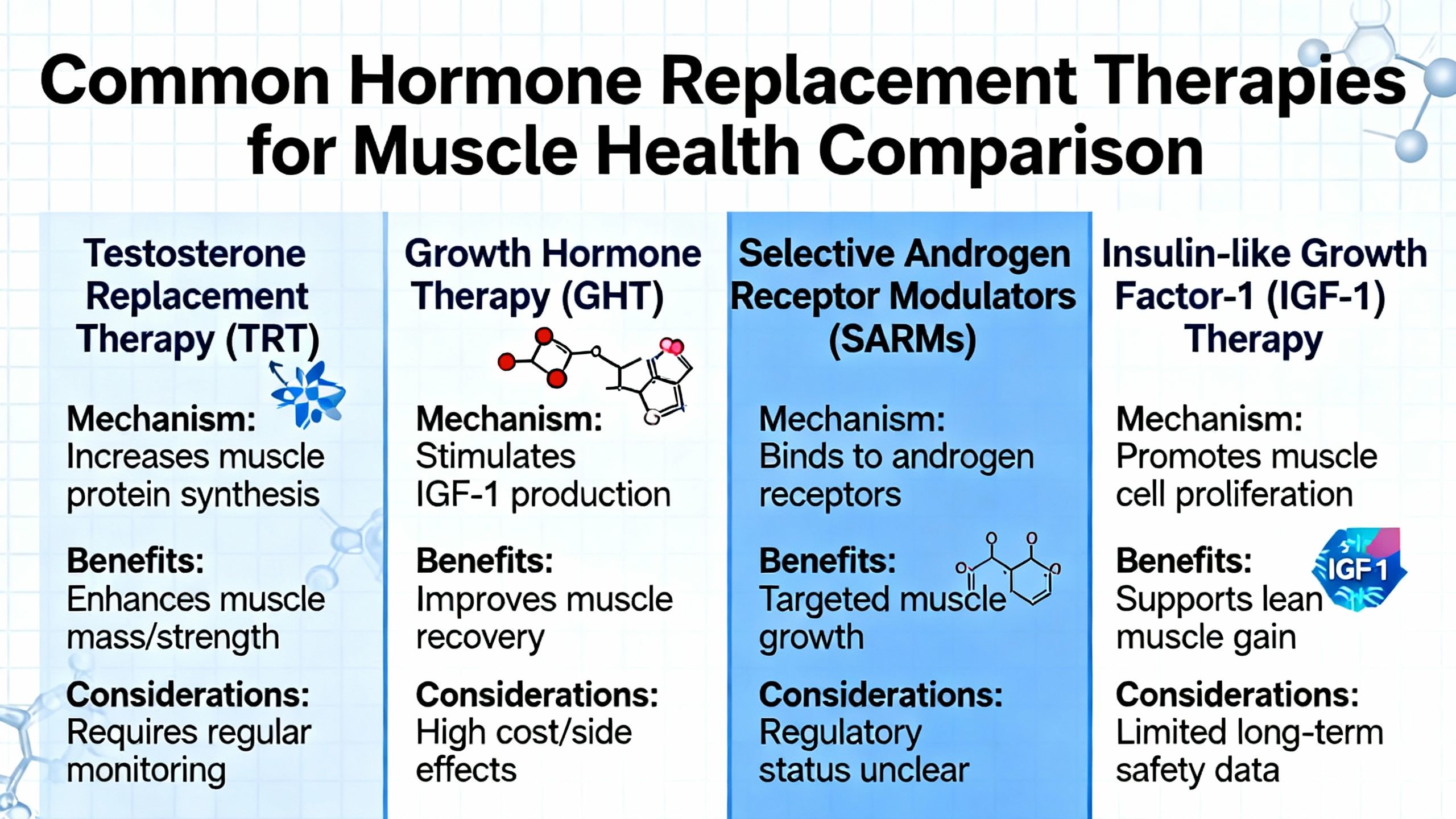
Comparison with Other Muscle-Preserving Approaches
Testosterone therapy is one of several interventions aimed at preventing or reversing age-related muscle loss:
- Peptide therapies: Early-stage alternatives like BPC-157 and MOTS-c show potential but lack robust human data.
- Selective androgen receptor modulators (SARMs): Some agents, like ostarine, show anabolic effects with fewer androgenic side effects but are not approved for general clinical use.
- Nutritional and exercise therapies: Remain first-line for all aging adults.
Summary: Should Aging Adults Consider Testosterone Therapy for Muscle Health?
Testosterone therapy can provide modest improvements in muscle mass and strength for aging adults—primarily in those with proven low levels and significant weakness or frailty. However, benefits must be carefully balanced against potential risks and side effects, especially regarding cardiovascular and prostate health. Routine screening, individualized dosing, and continuous monitoring are essential.
- Testosterone therapy aging research supports its selective use under specialist supervision.
- Do not use testosterone therapy for general anti-aging or without clear medical indication.
- Combine with exercise and nutrition for optimal benefit.
Always consult an endocrinologist or qualified healthcare provider for personalized assessment and management.
Studies / References
- Effects of testosterone supplementation for 3 years on muscle performance and physical function in older men
Large randomized controlled trial showing modest increases in lean body mass, muscle power, and physical function with longer-term testosterone use vs placebo.
https://pubmed.ncbi.nlm.nih.gov/27754805/ - Effects of testosterone supplementation on functional mobility, body composition, and quality of life in older men (JAMA-registered RCT)
This placebo-controlled trial found increases in lean body mass but mixed effects on functional mobility and strength.
https://jamanetwork.com/journals/jama/fullarticle/1149440 - Testosterone treatment increases muscle mass but mixed results on physical performance (meta-analysis/systematic review)
A broader evidence review/meta-analysis of multiple testosterone trials confirming consistent lean mass effects but inconsistent strength/function outcomes.
https://pubmed.ncbi.nlm.nih.gov/33045359/ - Transdermal testosterone increases muscle and decreases fat mass in healthy older men with low-normal testosterone
A randomized clinical study in elderly men showing lean mass gain and body composition changes.
https://pubmed.ncbi.nlm.nih.gov/25637335/ - Narrative review: Testosterone therapy, sarcopenia, and frailty in older men
A recent narrative review summarizing human evidence linking testosterone replacement with muscle outcomes and frailty measures.
https://pmc.ncbi.nlm.nih.gov/articles/PMC9605266/