Aging is accompanied by a remarkable array of hormonal changes that affect nearly every system in the body—none perhaps more visibly than our muscles. Loss of strength and muscle mass, clinically known as sarcopenia, is one of the primary drivers of frailty and disability in older adults, with far-reaching impacts on independence and quality of life. Understanding how hormonal changes during aging contribute to muscle degeneration is central to preventing, managing, and even reversing age-related muscle loss. This article explores the core mechanisms, human research, and promising evidence-based solutions targeting these hormonal shifts.
Introduction: The Biology of Hormonal Changes in Aging
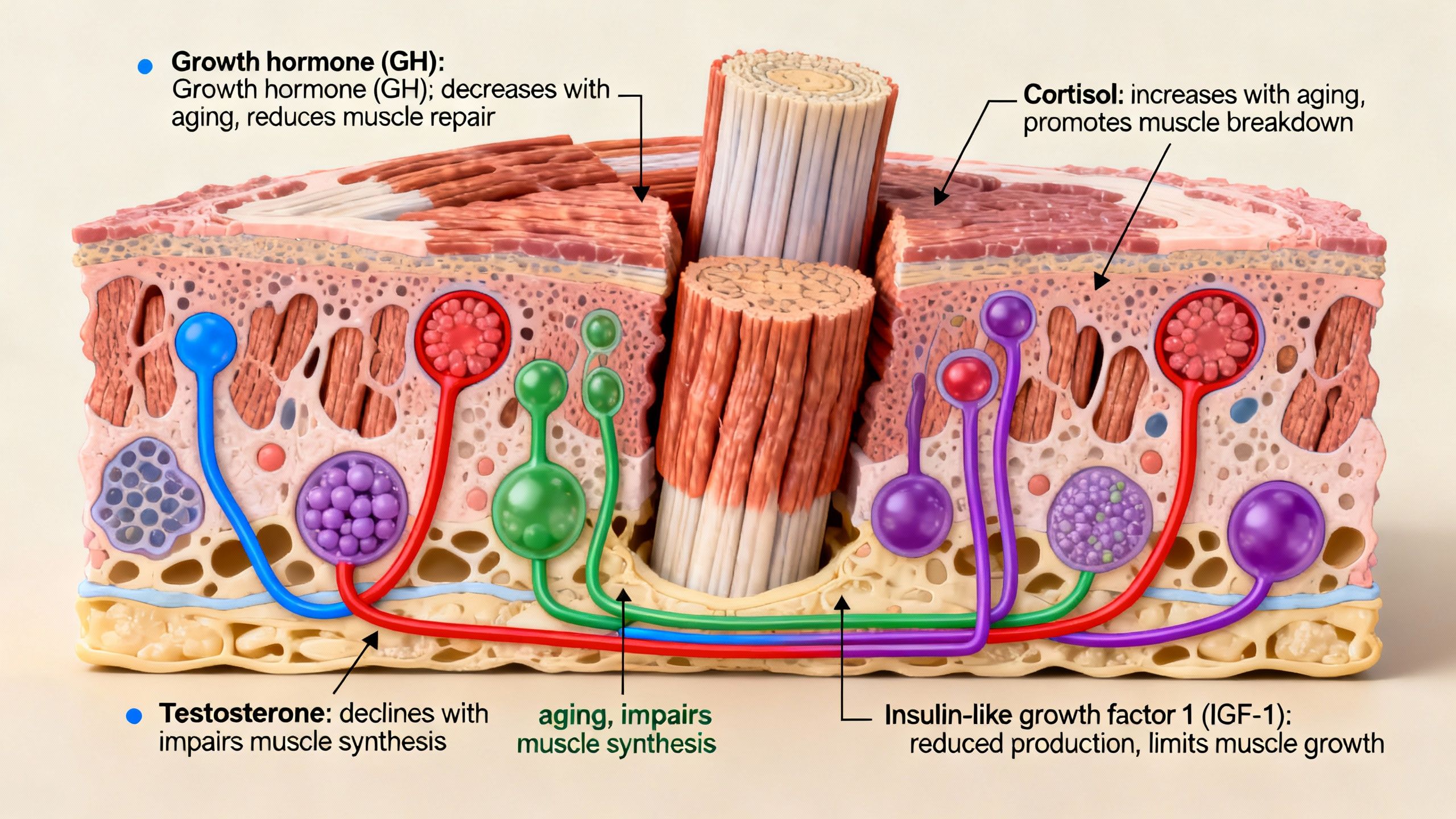
As we age, our body’s normal hormonal patterns shift dramatically. These changes influence muscle metabolism, repair, and growth. Some of the key hormones involved include:
- Testosterone: Governs muscle protein synthesis, essential for growth and maintenance
- Estrogen: Plays an important role in muscle strength, particularly in women
- Insulin-like Growth Factor 1 (IGF-1): Promotes muscle growth and regeneration
- Growth Hormone: Aids in tissue repair
- Cortisol: Chronic elevation can accelerate muscle breakdown
Disruption in the availability or effectiveness of these hormones drives much of the musculoskeletal decline seen in elderly populations.
Hormonal Changes in Aging: What Happens to Our Muscles?
The process of sarcopenia is multifactorial but strongly influenced by changing hormone levels. Key age-related hormonal changes include:
- Declining testosterone in men
- Sharp drop in estrogen after menopause in women
- Decreased secretion of growth hormone and IGF-1
Effects of Testosterone Decline on Muscle Mass with Aging
Testosterone slowly declines in men from about age 30 onward, with average losses of 1–2% per year. This reduction is linked to:
- Lower muscle protein synthesis rates
- Reduced muscle fiber size and number
- Impaired responses to exercise
- Higher risk of frailty and sarcopenia
Estrogen Decline and Muscle Weakness After Menopause
Women experience an abrupt fall in estrogen during the menopausal transition. Consequences include:
- Decreased muscle strength and power
- Increased difficulty maintaining physical function
- Higher susceptibility to muscle degeneration and impaired recovery
Growth Hormone/IGF-1 Changes in Muscle Aging
Both growth hormone (GH) and IGF-1 decline with age, leading to:
- Slower muscle regeneration
- Reduced satellite cell activation, necessary for muscle repair
- Increased fat infiltration into muscle
The Mechanisms: How Hormonal Changes Drive Sarcopenia
Let’s dive into the cellular and molecular level for how hormone changes specifically fuel muscle degeneration:
Testosterone
- Stimulates muscle protein synthesis via androgen receptors
- Promotes differentiation of muscle stem cells
- Enhances neuromuscular function for maximal strength
Estrogen
- Modulates muscle metabolism and mitochondrial health
- Protects against oxidative stress in muscle cells
- Supports muscle satellite cell pool maintenance
IGF-1 & Growth Hormone
- Activate the Akt/mTOR pathway for protein synthesis
- Promote muscle cell differentiation and growth
- Suppress muscle protein breakdown
Cortisol
- Chronic elevation (from stress/illness) increases muscle protein degradation
- Can exacerbate muscle loss when balanced by lower anabolic hormones
Individual Variability and Risk Factors
Not everyone experiences hormonal changes or muscle loss at the same rate. Influencing factors include:
- Genetics (androgen receptor variations, estrogen metabolism genes)
- Physical activity (resistance exercise can partially offset hormone decline)
- Nutrition (adequate protein, vitamin D, omega-3s)
- Comorbidities (diabetes, cardiovascular disease)
Key Point: Sarcopenia is preventable and partially reversible with the right strategies, even as hormones naturally decline.

Research-Backed Medical and Lifestyle Interventions
Addressing muscle loss in aging requires a multi-faceted approach. Let’s examine what the evidence tells us:
1. Resistance Exercise: The Cornerstone
- Strongest evidence for maintaining/increasing muscle mass
- Recommended: 2–3 sessions/week focusing on major muscle groups
- Benefits all genders, even well into the 80s and beyond
2. Protein and Nutrition Optimization
- Older adults need higher protein intake to support muscle anabolism (1.2–1.5 g/kg body weight)
- Leucine-rich sources may be especially helpful
- Vitamin D and omega-3s also support muscle health
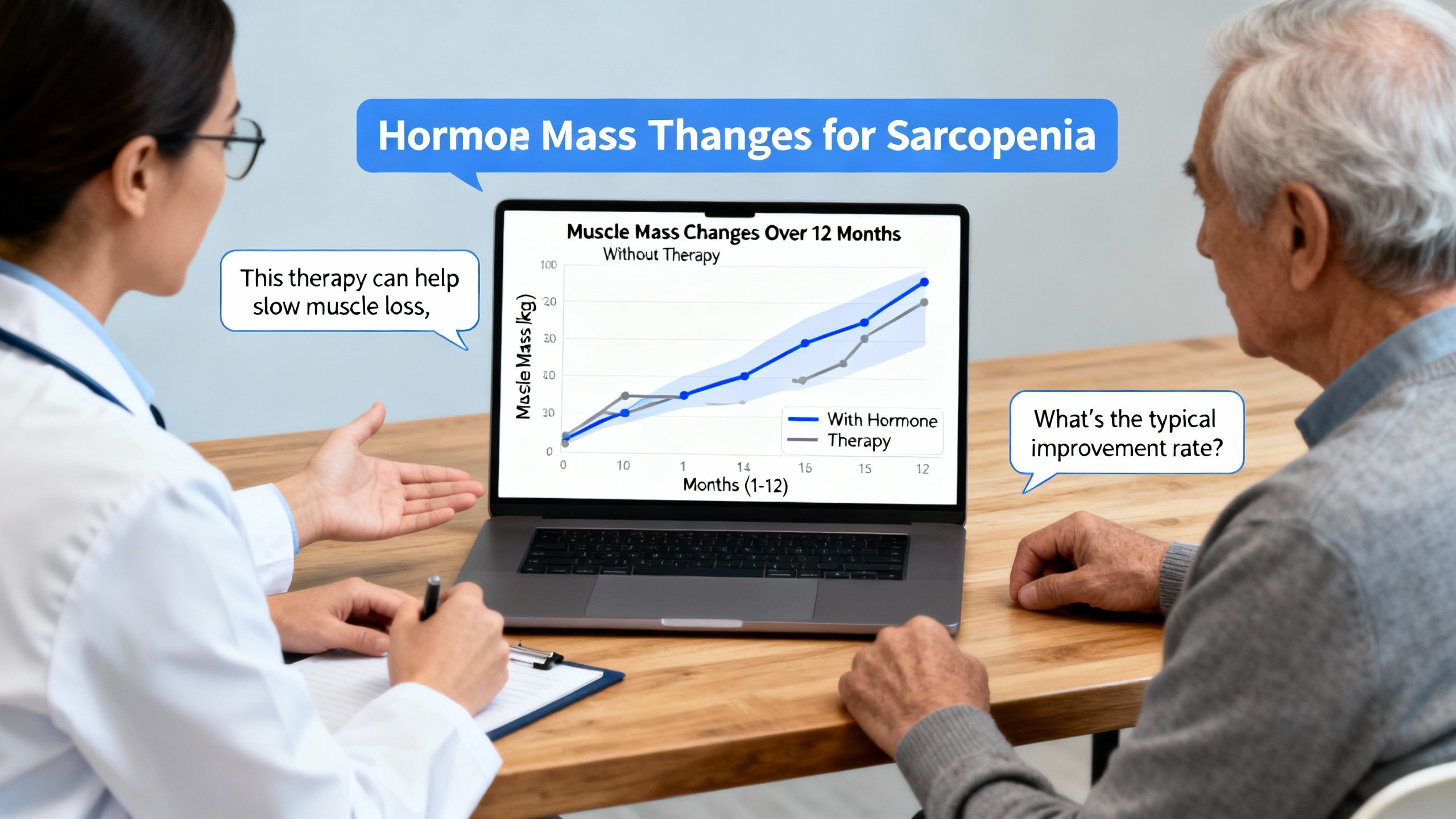
3. Testosterone Replacement in Older Men
- Testosterone Replacement Therapy (TRT) may benefit selected men with clear testosterone deficiency AND symptoms
- Demonstrated improvements in muscle mass, strength, and physical function in several trials
- Safety concerns: Polycythemia, cardiovascular risk, prostate considerations
- Not for everyone — specialist evaluation is required
4. Estrogen/SERM Therapy in Women
- Traditional hormone therapy post-menopause may mitigate muscle loss, but long-term risks (breast cancer, clotting)
- Selective Estrogen Receptor Modulators (SERMs): Options like raloxifene, tamoxifen, and bazedoxifene show promise for muscle protection with lower risk profiles
- Ongoing studies are exploring effects on muscle function, bone health, and safety
5. Growth Hormone/IGF-1 Modulation
- Direct supplementation is controversial (side effects, lack of long-term benefit)
- Focus is shifting to stimulating natural GH/IGF-1 release through resistance exercise and optimal sleep
Compound Focus: SERMs, Raloxifene, Tamoxifen, Bazedoxifene, Testosterone
These compounds intervene in hormone pathways with varying degrees of efficacy and safety.
SERMs in Older Adults
SERMs bind to estrogen receptors, either mimicking or blocking estrogen’s effects depending on the tissue. In muscle, SERMs may:
- Preserve or enhance muscle mass and strength post-menopause
- Lower fracture risk by maintaining both bone and muscle density
- Offer similar benefits to estrogen therapy, but with less risk of malignancy/vascular events
Raloxifene and bazedoxifene are best-studied for osteoporosis, but new research is exploring their muscle benefits.
Raloxifene
- Evidence suggests improved muscle quality and reduced falls in postmenopausal women
- Raloxifene is commonly prescribed for bone health; muscle benefits are an emerging area
Tamoxifen
- Used in breast cancer treatment; shows some muscle protective effects, though benefits are less clear compared to other SERMs
Bazedoxifene
- Recent studies indicate potential for muscle and bone protection, especially as part of combination therapy (with conjugated estrogens)
Testosterone
- For men with clinical hypogonadism: increases muscle mass and strength
- Not approved broadly for age-related decline without confirmed deficiency
- Individual risk/benefit assessment is essential
Caveats, Safety, and Clinical Considerations
- Hormone therapies carry risks and are not appropriate for everyone. Screening for cancers, cardiovascular status, and prostatic/gynaecological health is mandatory.
- Lifestyle interventions (diet, resistance training) should be first-line.
- Individual response, side effects, and long-term efficacy vary.
Consultation with endocrinology or geriatric specialists is always required before any hormonal therapy.
Mechanisms of Muscle Preservation and Recovery
How do these interventions actually work to preserve muscle?
- Resistance training plus protein: Stimulates muscle protein synthesis through mTOR and satellite cell pathways
- Testosterone/SERMs: Activate muscle androgen or estrogen receptors, upregulating anabolic signaling; can enhance satellite cell proliferation
- Optimal nutrition: Provides building blocks and cofactors for muscle repair
Practical Applications and Prevention of Sarcopenia
Here’s how you can apply this evidence in real-world settings:
- Start or continue resistance training after age 50—there is NO age limit for muscle gain
- Ensure daily protein intake exceeds 1.2 g/kg
- Use hormone therapies only under medical guidance and with regular monitoring
- Screen for vitamin D deficiency and treat if needed
- Consider SERM therapy if postmenopausal and at risk for osteoporosis/sarcopenia
Frequently Asked Questions
Can hormonal changes be ‘reversed’?
Hormone decline with age is natural, but effects can often be mitigated—not always fully reversed. Individualized therapy offers the best outcomes.
How long does it take to see improvement?
With resistance training and optimal nutrition, improvements in strength can occur in as little as 8–12 weeks. Hormone therapies may take 3–6 months for maximal effect.
Are there downsides to hormone therapy for sarcopenia?
Yes—risks include cardiovascular events, cancer risk (breast/prostate), and possible metabolic changes. All therapies should be supervised.
Table: Key Hormonal Shifts in Aging and Interventions
| Hormone | Change With Age | Muscle Effect | Evidence-Based Interventions |
|---|---|---|---|
| Testosterone | Decreases | Lower mass/strength | Resistant exercise, replacement therapy* |
| Estrogen | Decreases | Weaker muscle, more fat | SERMs, HRT* (case-by-case) |
| Growth Hormone | Decreases | Slower repair | Exercise, sleep |
| IGF-1 | Decreases | Atrophy, weaker repair | Exercise, nutrition |
| Cortisol | May increase | Catabolism (breakdown) | Stress management, healthy lifestyle |
*With clinical indications and specialist oversight
Studies / References
- Testosterone Replacement in Older Men
One randomized controlled trial in men over 65 compared testosterone replacement to placebo over 12 months. Those receiving testosterone experienced increased muscle mass and strength, but with a higher rate of erythrocytosis; effects diminished after therapy stopped.
https://pubmed.ncbi.nlm.nih.gov/20601412/ - Raloxifene in Postmenopausal Women
A two-year study in postmenopausal women assessed raloxifene versus placebo. Raloxifene led to modest increases in muscle quality and reductions in falls, but muscle strength increase was not significant. It was generally safe but did carry a slightly increased risk of thromboembolic events.
https://pubmed.ncbi.nlm.nih.gov/19884264/ - Resistance Training and Muscle Preservation
An observational cohort tracked physical activity and muscle mass in adults over 70. Those consistently engaging in resistance training had significantly less muscle mass loss, regardless of baseline hormone levels.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7140321/ - Bazedoxifene with Conjugated Estrogen
A randomized trial of bazedoxifene with conjugated estrogen in women showed improvements in both bone density and markers of muscle health over 18 months, with fewer side effects than traditional hormone therapy; data on long-term muscle outcomes is still emerging.
https://www.tandfonline.com/doi/full/10.2147/tcrm.s3476 - Meta-Analysis of Hormone Therapy and Exercise for Sarcopenia
A meta-analysis of hormone therapy and exercise interventions for sarcopenia found the greatest effect on muscle strength and mass when both were combined, but variability in results and higher adverse event rates with hormones alone.
https://www.mdpi.com/2077-0383/11/20/6202
Conclusion: Future Directions and Clinical Takeaways
Hormonal changes during aging are a major—though not inevitable—cause of muscle degeneration and frailty in older adults. The integration of resistance exercise, optimal nutrition, and selective use of medical therapies (such as SERMs or testosterone in carefully chosen individuals) provides the most effective strategy for preserving independence and quality of life.
Ongoing research is rapidly deepening our understanding of age-related hormonal changes and muscle loss. Clinicians and patients alike should emphasize proven interventions while remaining aware of evolving evidence around newer therapies.
Key Takeaway: With a proactive, evidence-based approach, the negative impact of hormonal changes on muscle health during aging can be minimized, enabling healthy, active aging for years to come.




